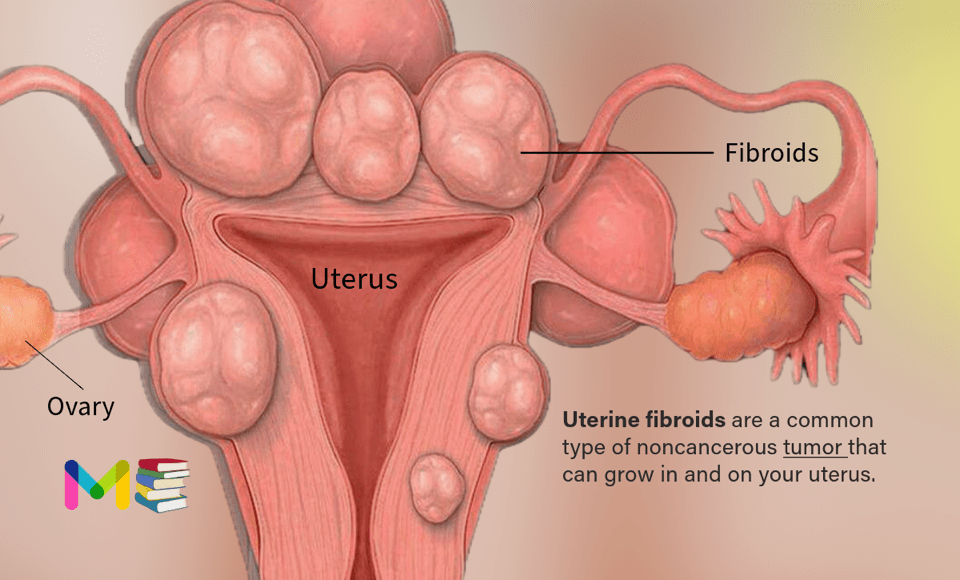
Uterine fibroids (also called leiomyomas) are a common type of noncancerous tumor. They are growths made of smooth muscle cells and fibrous connective tissue.
These growths develop in the uterus and appear alone or in groups. They range in size, from as small as a grain of rice to as big as a melon.
In some cases, fibroids can grow into the uterine cavity or outward from the uterus on stalks. In extreme cases, some fibroids grow large enough to fill the pelvis or stomach area. They can make a person look pregnant. Fibroids aren’t linked with a higher risk of types of cancer in the uterus either.
Many people have uterine fibroids sometime during their lives. But you might not know you have them, because they often cause no symptoms. Your health care professional may just happen to find fibroids during a pelvic exam or pregnancy ultrasound. People who haven’t had their first period (menstruation) yet typically don’t have fibroids.
Uterine fibroids can cause a variety of symptoms like pain and heavy, irregular vaginal bleeding. Sometimes, a person has no symptoms and is unaware they have fibroids. Treatment for fibroids typically depends on the symptoms.
According to the U.S. Department of Health and Human Services, around 20% to 80% of women have them by the age of 50 years old. However, most people don’t have any symptoms and may never know they have fibroids.
Fibroids are also known by the following names:
- uterine fibroids
- fibromas
- myomas
- leiomyomas
- uterine myomas
Pregnancy and fibroids
Often, fibroids don’t interfere with getting pregnant. But some fibroids, especially the submucosal kind, could cause infertility or pregnancy loss.
Fibroids also may raise the risk of certain pregnancy complications. These include:
- Placental abruption, when the organ that brings oxygen and nutrients to the baby, called the placenta, separates from the inner wall of the uterus.
- Fetal growth restriction, when an unborn baby doesn’t grow as well as expected.
- Preterm delivery, when a baby is born too early, before the 37th week of pregnancy.
Table of Contents
Key points on Uterine fibroids
- People who haven’t had their first period (menstruation) yet, typically don’t have fibroids.
- Uterine fibroids are an extremely common condition in which solid tumors develop in the uterus.
- Fibroids are not cancerous and do not increase the risk for uterine cancer.
- It is not known what causes fibroids, but studies suggest genetics and prolonged exposure to estrogen may increase your risk of developing fibroids.
- Symptoms can include heavy and prolonged periods, bleeding between periods, pressure in the abdomen and pelvic pain.
- Fibroids are most often found during a routine pelvic exam or incidentally noted on imaging. If treatment is needed, it may include medications or surgery.
Size of uterine fibroids
Fibroids can grow as a single nodule (one growth) or in a cluster. Clusters of fibroids can range in size from 1 millimeter to more than 20 centimeters (8 inches) in diameter or even larger. For comparison, fibroids can be as small as a seed or get as large as a watermelon. These growths can develop within the wall of your uterus, inside the main cavity of your uterus or on the outer surface of your uterus.
Types of uterine fibroids
There are various types of fibroids. The types differ depending on their location in or on the uterus.
- Intramural fibroids: Intramural fibroids are the most common type. They appear within the muscular wall of the uterus. Intramural fibroids may grow larger and can stretch your uterus.
- Subserosal fibroids: Subserosal fibroids form on the outside of your uterus, which is called the serosa. They may grow large enough to make your uterus appear bigger on one side.
- Pedunculated fibroids: Subserosal fibroids can develop a stem, a slender base that supports the tumor. When they do, they’re known as pedunculated fibroids.
- Submucosal fibroids: These types of tumors develop in the myometrium, the middle muscle layer of your uterus. Submucosal tumors aren’t as common as other types.
- Cervical fibroids: Cervical fibroids develop on the cervix, which connects the uterus to the vagina. They’re also rare.
Symptoms of uterine fibroids
It is common that women who have fibroids do not experience any noticeable symptoms. Other women with fibroids experience severe symptoms that interfere with their daily lives. Common fibroid symptoms include:
- Heavy or prolonged periods
- Bleeding between periods
- Abdominal discomfort and/or fullness
- A feeling of fullness in your lower belly (abdomen)/bloating
- Long-term (chronic) vaginal discharge
- Pelvic pain
- Lower back pain
- Bladder symptoms, such as frequent urination or difficulty emptying the bladder
- Bowel symptoms, such as constipation or excessive straining with bowel movements
- Infertility
- Complications during pregnancy
- Pain during intercourse
- Increased abdominal distention (enlargement), causing your abdomen to look pregnant.
In rare cases, women with fibroids need emergency treatment. You should seek emergency care if you have sharp, sudden pain in the abdomen that is unrelieved with pain medication, or severe vaginal bleeding with signs of anemia such as lightheadedness, extreme fatigue and weakness.
Causes of uterine fibroids
The exact cause of uterine fibroids isn’t clear. But study suggests the following factors:
- Gene changes. Many fibroids contain changes in genes that differ from those in typical uterine muscle cells.
- Family history: Fibroids may run in the family. If your mother, sister, or grandmother has a history of this condition, you may develop it as well.
- Hormones. Two hormones called estrogen and progesterone cause the tissue the lines the inside of the uterus to thicken during each menstrual cycle to prepare for pregnancy. These hormones also seem to help fibroids grow.Fibroids contain more cells that estrogen and progesterone bind to than do typical uterine muscle cells. Fibroids tend to shrink after menopause due to a drop in hormone levels.
- Other growth factors. Substances that help the body maintain tissues, such as insulin-like growth factor, may affect fibroid growth.
- Extracellular matrix (ECM). This material makes cells stick together, like mortar between bricks. ECM is increased in fibroids and makes them fibrous. ECM also stores growth factors and causes biologic changes in the cells themselves.
Doctors believe that uterine fibroids may develop from a stem cell in the smooth muscular tissue of the uterus. A single cell divides over and over. In time it turns into a firm, rubbery mass distinct from nearby tissue.
The growth patterns of uterine fibroids vary. They may grow slowly or fast. Or they might stay the same size. Some fibroids go through growth spurts, and some shrink on their own.
Fibroids that form during pregnancy can shrink or go away after pregnancy, as the uterus goes back to its usual size.
Symptoms and causes of ectopic pregnancy
Risk factors of uterine fibroids
There are several risk factors that can play a role in your chances of developing fibroids. These can include:
- Race. All people of reproductive age who were born female could develop fibroids. But Black people are more likely to have fibroids than are people of other racial groups. Black people have fibroids at younger ages than do white people. They’re also likely to have more or larger fibroids, along with worse symptoms, than do white people.
- Obesity and a higher body mass index (BMI).
- Family history of fibroids.
- Not having children.
- Early onset of menstruation (getting your period at a young age).
- Late age for menopause.
Complications of uterine fibroids
Most uterine fibroids don’t cause serious complications. However, the most common complications of fibroids are:
- Pain that becomes unmanageable.
- Swelling of your abdomen or pelvic area.
- Excessive bleeding.
- Anemia.
- Infertility (this is rare).
Anemia is a condition that happens when your body doesn’t have enough healthy red blood cells to carry oxygen to your organs. Anemia can happen to people who have frequent or extremely heavy periods. Fibroids can cause your periods to be very heavy or for you to even bleed between periods. Talk to your healthcare provider if you’re experiencing symptoms of anemia while you have fibroids.
Risk factors and complications of Endometriosis
Prevention of uterine fibroids
In general, you can’t prevent fibroids. You can reduce your risk by maintaining a healthy body weight and getting regular pelvic exams. If you have small fibroids, develop a plan with your healthcare provider to monitor them.
Researchers continue to study the causes of fibroid tumors. More research is needed on how to prevent them, though. It might not be possible to prevent uterine fibroids. But only a small percentage of these tumors need treatment.
Some research suggests that birth control pills or long-acting progestin-only contraceptives may lower the risk of fibroids. But using birth control pills before the age of 16 may be linked with a higher risk.
Diagnosis of uterine fibroids
In many cases, a healthcare provider discovers uterine fibroids during a pelvic exam. Quite often, heavy bleeding and other related symptoms may alert your provider to consider fibroids as a part of the diagnosis. There are several tests that can be done to confirm fibroids and determine their size and location. These tests can include:
- Ultrasound: This test uses sound waves to get a picture of your uterus. It can confirm that you have fibroids, and map and measure them. A doctor or technician moves the ultrasound device, called a transducer, over your stomach area. This is called a transabdominal ultrasound. Or the device is placed inside your vagina to get images of your uterus. This is called a transvaginal ultrasound.
- Lab tests: If you have irregular menstrual bleeding, you may need blood tests to look for possible causes of it. These might include a complete blood count to check for anemia due to ongoing blood loss. Other blood tests can search for bleeding disorders or thyroid problems.
- Ultrasonography: This noninvasive imaging test creates a picture of your internal organs with sound waves.
- Magnetic resonance imaging (MRI): This test creates detailed images of your internal organs by using magnets and radio waves.
- Computed tomography (CT) scan: A CT scan uses X-ray images to make a detailed image of your internal organs from several angles.
- Hysteroscopy: During a hysteroscopy, your provider will use a device called a scope (a thin, flexible tube with a camera on the end) to look at fibroids inside your uterus. The scope is passed through your vagina and cervix and then moved into your uterus.
- Hysterosalpingography (HSG): This is a detailed X-ray where your provider injects contrast material and then takes X-rays of your uterus.
- Sonohysterography: In this imaging test, your provider places a small catheter in your vagina and then injects saline into your uterus. This extra fluid helps to create a clearer image of your uterus than you would see during a standard ultrasound.
- Laparoscopy: During this test, your provider will make a small cut (incision) in your lower abdomen. A thin and flexible tube with a camera on the end will be inserted to look closely at your internal organs.
- Hysterosonography: Hysterosonography (his-tur-o-suh-NOG-ruh-fee) uses sterile salt water called saline to expand the space inside the uterus, called the uterine cavity. This makes it easier to get images of submucosal fibroids and the lining of the uterus if you’re trying to get pregnant or if you have heavy menstrual bleeding. Another name for hysterosonography is a saline infusion sonogram.
Prevention and diagnosis of adenomyosis
Treatment of uterine fibroids
There’s no single best treatment for uterine fibroids. Many treatment choices exist. If you have symptoms, talk with your care team about ways to get relief.
Watchful waiting
Many people with uterine fibroids have no symptoms. Or they have mildly annoying symptoms that they can live with. If that’s the case for you, watchful waiting could be the best option.
Fibroids aren’t cancer. They rarely interfere with pregnancy. They often grow slowly, or not at all, and tend to shrink after menopause, when levels of reproductive hormones drop.
Medications
Medicines for uterine fibroids target hormones that control the menstrual cycle. They treat symptoms such as heavy menstrual bleeding and pelvic pressure. They don’t get rid of fibroids, but they may shrink them. Medicines include:
- Gonadotropin-releasing hormone (GnRH) agonists. These treat fibroids by blocking the body from making the hormones estrogen and progesterone. This puts you into a temporary menopause-like state. As a result, menstrual periods stop, fibroids shrink and anemia often gets better.GnRH agonists include leuprolide (Lupron Depot, Eligard, others), goserelin (Zoladex) and triptorelin (Trelstar, Triptodur Kit).Many people have hot flashes while using GnRH agonists. Often, these medicines are used for no more than six months. That’s because symptoms return when the medicine is stopped, and long-term use can cause loss of bone. Sometimes, GnRH agonists are taken with low-dose estrogen or progestin. You might hear this called add-back therapy. It can ease side effects, and it might allow you to take GnRH agonists up to 12 months.Your doctor may prescribe a GnRHagonist to shrink the size of your fibroids before a planned surgery. Or you might be prescribed this medicine to help transition you into menopause.
- Gonadotropin-releasing hormone (GnRH) antagonists. These medicines can treat heavy menstrual bleeding in people with uterine fibroids who haven’t gone through menopause. But they don’t shrink fibroids. GnRHantagonists can be used for up to two years. Taking them along with add-back therapy can lessen side effects such as hot flashes and bone loss. Sometimes, low-dose estrogen or progestin are already included in these medicines.GnRH antagonists include elagolix (Oriahnn) and relugolix (Myfembree).
- Progestin-releasing intrauterine device (IUD). A progestin-releasing IUD can relieve heavy bleeding caused by fibroids. It only relieves symptoms, though. It doesn’t shrink fibroids or make them go away. It also prevents pregnancy.
- Tranexamic acid (Lysteda, Cyklokapron). This nonhormonal medicine can ease heavy menstrual periods. You take it only on heavy bleeding days.
- Other medicines. Your doctor might recommend other medicines. For example, low-dose birth control pills can help control menstrual bleeding. But they don’t reduce fibroid size.Medicines called nonsteroidal anti-inflammatory drugs (NSAIDs) may help relieve pain tied to fibroids, but they don’t reduce bleeding caused by fibroids. NSAIDs aren’t hormonal medicines. Examples include ibuprofen (Advil, Motrin IB, others) and naproxen sodium (Aleve). Your doctor also may suggest that you take vitamins and iron if you have heavy menstrual bleeding and anemia.
Noninvasive procedure
A noninvasive treatment doesn’t involve surgical cuts called incisions. It also doesn’t involve tools being placed in the body. With uterine fibroids, a procedure called MRI-guided focused ultrasound surgery (FUS) is:
- A noninvasive treatment option that preserves the uterus. It’s done on an outpatient basis, meaning you don’t have to spend the night at the hospital afterward.
- Done while you’re inside an MRI scanner equipped with a high-energy ultrasound device for treatment. The images give your doctor the precise location of the uterine fibroids. When the location of the fibroid is targeted, the ultrasound device focuses sound waves into the fibroid to heat and destroy small areas of fibroid tissue.
- Newer technology, so researchers are learning more about the long-term safety and effectiveness. But so far data collected show that FUS for uterine fibroids is safe and works well. Still, it might not improve symptoms as much as a slightly more invasive procedure called uterine artery embolization could.
Minimally invasive medical procedures
These procedures use no cuts or small cuts. They’re linked with faster recovery times and fewer complications compared with traditional open surgery. Minimally invasive treatments for uterine fibroids include:
- Uterine artery embolization. Small particles called embolic agents are injected into the arteries that supply the uterus with blood. The particles cut off blood flow to fibroids, causing them to shrink and die.This technique can help shrink fibroids and relieve the symptoms they cause. Complications may happen if the blood supply to your ovaries or other organs is reduced. But research shows that complications are similar to surgical fibroid treatments. And the risk of needing a blood transfusion is lower.
- Radiofrequency ablation. In this procedure, heat from radiofrequency energy destroys uterine fibroids and shrinks the blood vessels that feed them. This can be done through small cuts in the stomach area, a type of surgery called laparoscopy. It also can be done through the vagina, called a transvaginal procedure, or through the cervix, called a transcervical procedure.With laparoscopic radiofrequency ablation, your doctor makes two small cuts in the abdomen. A slim viewing tool with a camera at the tip, called a laparoscope, is placed through the cuts. Using the camera and an ultrasound tool, your doctor finds fibroids to be treated.After finding a fibroid, your doctor uses a device to send small needles into the fibroid. The needles heat up the fibroid tissue and destroy it. The destroyed fibroid changes right away. For instance, it goes from being hard like a golf ball to being soft like a marshmallow. During the next 3 to 12 months, the fibroid continues to shrink, and symptoms get better.Laparoscopic radiofrequency ablation is also known as the Acessa procedure or Lap-RFA. Because there’s no cutting of uterine tissue, doctors consider Lap-RFA a less invasive treatment than surgeries such as a hysterectomy and a myomectomy. Most people who have the procedure get back to regular activities within a few days.The transcervical, or through the cervix, approach to radiofrequency ablation is called Sonata. It also uses ultrasound guidance to locate fibroids.
- Laparoscopic or robotic myomectomy. In a myomectomy, your surgeon removes the fibroids and leaves the uterus in place.If the fibroids are few in number, you and your doctor may opt for a laparoscopic procedure. This uses slender instruments placed through small cuts in the abdomen to remove the fibroids from the uterus.Sometimes, a robotic system is used for the laparoscopic procedure. Your doctor views your stomach area on a monitor using a small camera attached to one of the instruments. Robotic myomectomy gives your surgeon a magnified, 3D view of your uterus. This can make the procedure more precise than is possible using some other techniques.Larger fibroids can be removed through smaller cuts by breaking them into pieces with a device that cuts tissue. This is called morcellation. It can be done inside a surgical bag to lower the risk of spreading any cancer cells that doctors hadn’t expected to find. Or it can be done by extending one incision to remove the fibroids without morcellation.
- Hysteroscopic myomectomy. This procedure may be an option if the fibroids are inside the uterus, also called submucosal fibroids. The fibroids are removed using tools placed through the vagina and cervix into the uterus.
- Endometrial ablation. This procedure can reduce heavy menstrual flow. A device that’s inserted into the uterus gives off heat, microwave energy, hot water, cold temperature or an electric current. This destroys the tissue that lines the inside of the uterus.You aren’t likely to get pregnant after endometrial ablation. But it’s a good idea to take birth control to prevent a fertilized egg from forming in a fallopian tube, called an ectopic pregnancy. Without treatment, the growing tissue might cause life-threatening bleeding.
With any procedure that doesn’t remove the uterus, there’s a risk that new fibroids could grow and cause symptoms.
Traditional surgical procedures
Options for traditional open surgeries that use a larger incision include:
- Abdominal myomectomy. This type of surgery removes fibroids through a larger cut in the stomach area, also called the abdomen. Your doctor may recommend it if you have more than one fibroid, very large fibroids or very deep fibroids.Many people who are told that hysterectomy is their only option can have an abdominal myomectomy instead. Scarring after surgery can lower the chances of being able to get pregnant in the future, though.
- Hysterectomy. This surgery removes the uterus. It remains the only proven permanent solution for uterine fibroids.Hysterectomy ends your ability to bear children. If you also decide to have your ovaries removed, the surgery brings on menopause. You’ll then choose whether to take hormone replacement therapy, which is medicine that can ease menopause side effects such as hot flashes. Most people with uterine fibroids may be able to choose to keep their ovaries.
Morcellation during fibroid removal
Morcellation is a process of breaking fibroids into smaller pieces. It can raise the risk of spreading cancer if a cancerous tumor that hadn’t been found earlier gets broken up with morcellation during a myomectomy procedure. The risk can be lowered if:
- The surgical team looks into a person’s risk factors before surgery.
- The fibroid is broken up in a surgical bag during morcellation.
- The incision is expanded to remove a large fibroid without morcellation.
All myomectomies carry the risk of cutting into cancer that hasn’t been found. But younger people who haven’t reached menopause by and large have a lower risk of undiagnosed cancer than do people over the age of 50.
Also, complications during open surgery are more common than the chance of spreading an unsuspected cancer in a fibroid during a minimally invasive procedure. If your doctor is planning to use morcellation, ask the doctor to explain your risks before treatment.
For all procedures except hysterectomy, seedlings, tiny tumors that your doctor doesn’t detect during surgery, could one day grow and cause symptoms that need treatment. Often, this is called the recurrence rate. New fibroids also can form, and these may need treatment.
Also, some procedures may only treat some of the fibroids present at the time of treatment. These include laparoscopic or robotic myomectomy, radiofrequency ablation, and MRI-guided focused ultrasound surgery (FUS).
There can be risks to any treatment. Medications can have side effects and some may not be a good fit for you. Talk to your healthcare provider about all medications you may be taking for other medical conditions and your complete medical history before starting a new medication. If you experience side effects after starting a new medication, call your provider to discuss your options.
There are also risks involved in surgical treatment of fibroids. Any surgery places you at risk of infection and bleeding, and includes risks associated with anesthesia. An additional risk of fibroid removal surgery can involve future pregnancies. Some surgical options can prevent future pregnancies. Myomectomy is a procedure that only removes the fibroids, allowing for future pregnancies. However, people who’ve had a myomectomy may need to deliver future babies via C-section.
If you have fibroids and are experiencing infertility, consult a reproductive endocrinologist who specializes in treatment of women with fibroids. A fertility specialist can develop a treatment plan that maximizes your chances of a successful pregnancy. If surgery to treat fibroids is needed before pursuing fertility treatment, myomectomy is likely your best option.
- Medmichihealthcare New posts
- Read All causes of disease short notes
- Read All diagnosis of disease short notes
- Read All treatment of disease short notes
- Subscribe Medmichihealthcare YouTube channel
Discover more from Medmichihealthcare
Subscribe to get the latest posts to your email.