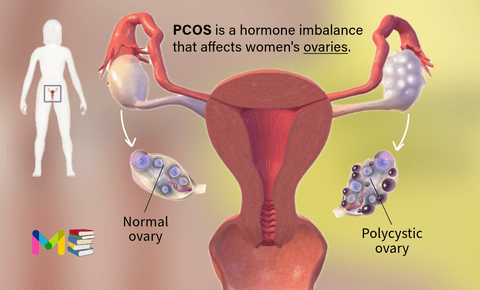
Polycystic ovary syndrome (PCOS) is a hormonal imbalance that occurs when your ovaries (the organ that produces and releases eggs) create excess hormones. It is a problem that occurs during the reproductive years.
Small follicle cysts (fluid-filled sacs with immature eggs) may be visible on your ovaries on ultrasound due to lack of ovulation (anovulation). However, despite the name “polycystic,” you don’t need to have cysts on your ovaries to have PCOS. The ovarian cysts aren’t dangerous or painful.
When small sacs of fluid develop along the outer edge of the ovary. The small fluid-filled cysts contain immature eggs. These are called follicles. The follicles fail to regularly release eggs.
If you have PCOS, you may not have periods very often. Or you may have periods that last many days. You may also have too much of a hormone called androgen in your body.
Ovulation occurs when a mature egg is released from an ovary. This happens so it can be fertilized by a male sperm. If the egg is not fertilized, it is sent out of the body during your period. In some cases, a woman doesn’t make enough of the hormones needed to ovulate. When ovulation doesn’t happen, the ovaries can develop many small cysts. These cysts make more androgens.
PCOS is one of the most common causes of infertility in women and people assigned female at birth (AFAB). It can also increase your risk of other health conditions. Your healthcare provider can treat PCOS based on your symptoms and if you wish to become pregnant.
PCOS also causes hair growth on the face and body, and baldness. And it can contribute to long-term health problems like diabetes and heart disease. The exact cause of PCOS is unknown. Early diagnosis and treatment along with weight loss may lower the risk of long-term complications.
Polycystic ovary syndrome is very common and up to 15% of women and people AFAB (assigned female at birth) of reproductive age have it.
Table of Contents
Key points about polycystic ovary syndrome
- PCOS is a very common hormone problem for women of childbearing age.
- Women with PCOS may not ovulate, have high levels of androgens, and have many small cysts on the ovaries.
- PCOS can cause missed or irregular menstrual periods, excess hair growth, acne, infertility, and weight gain.
- Women with PCOS may be at higher risk for type 2 diabetes, high blood pressure, heart problems, and endometrial cancer.
- The types of treatment for PCOS may depend on whether or not a woman plans to become pregnant. Women who plan to become pregnant in the future may take different kinds of medications.
Symptoms of polycystic ovary syndrome
Some women start seeing symptoms around the time of their first period. Others only discover they have PCOS after they’ve gained a lot of weight or they’ve had trouble getting pregnant. The most common signs and symptoms of PCOS include:
- Irregular periods: abnormal menstruation involves missing periods or not having a period at all. It may also involve heavy bleeding during periods.
- Heavy bleeding. The uterine lining builds up for a longer period of time, so the periods you do get can be heavier than normal.
- Headaches. Hormone changes can trigger headaches in some women.
- Abnormal hair growth: You may grow excess facial hair or experience heavy hair growth on your arms, chest and abdomen (hirsutism). This affects up to 70% of people with PCOS.
- Acne: PCOS can cause acne, especially on your back, chest and face. This acne may continue past your teenage years and may be difficult to treat.
- Obesity: Between 40% and 80% of people with PCOS have obesity and have trouble maintaining a weight that’s healthy for them.
- Darkening of the skin: You may get patches of dark skin, especially in the folds of your neck, armpits, groin (between the legs) and under your breasts. This is known as acanthosis nigricans.
- Cysts: Many people with PCOS have ovaries that appear larger or with many follicles (egg sac cysts) on ultrasound.
- Skin tags: Skin tags are little flaps of extra skin. They’re often found in your armpits or on your neck.
- Thinning hair: People with PCOS may lose patches of hair on their head or start to bald.
- Infertility: PCOS is the most common cause of infertility in people AFAB. Not ovulating regularly or frequently can result in not being able to conceive.
PCOS can disrupt the menstrual cycle, leading to fewer periods. Acne, hair growth, weight gain, and dark skin patches are other symptoms of the condition.
Causes of polycystic ovary syndrome
The exact cause of PCOS is unknown. There’s evidence that genetics play a role. Several other factors, most importantly obesity, also play a role in causing PCOS:
- Heredity. Research suggests that certain genes might be linked to PCOS. Having a family history of PCOS may play a role in developing the condition.
- Insulin resistance. Insulin is a hormone that the pancreas makes. It allows cells to use sugar, your body’s primary energy supply. If cells become resistant to the action of insulin, then blood sugar levels can go up. This can cause your body to make more insulin to try to bring down the blood sugar level. Too much insulin might cause your body to make too much of the male hormone androgen. You could have trouble with ovulation, the process where eggs are released from the ovary. One sign of insulin resistance is dark, velvety patches of skin on the lower part of the neck, armpits, groin or under the breasts. A bigger appetite and weight gain may be other signs.
- Excess androgen. With PCOS, the ovaries may produce high levels of androgen. Having too much androgen interferes with ovulation. This means that eggs don’t develop on a regular basis and aren’t released from the follicles where they develop. Excess androgen also can result in hirsutism and acne.
- Low-grade inflammation. White blood cells make substances in response to infection or injury. This response is called low-grade inflammation. Research shows that people with PCOS have a type of long-term, low-grade inflammation that leads polycystic ovaries to produce androgens. This can lead to heart and blood vessel problems.
People with PCOS have a hormonal imbalance that disrupts their menstrual cycle, ovulation and possibly, conception. These hormones are like an intricate web and the function of your reproductive system relies heavily on its balance. The hormones that play a role in PCOS are:
- Androgens (like testosterone and androstenedione).
- Luteinizing hormone (LH).
- Follicle-stimulating hormone (FSH).
- Estrogen.
- Progesterone.
- Insulin.
Polycystic ovary syndrome and Endometriosis
PCOS and endometriosis are different conditions, but both can cause ovarian cysts and infertility. Endometriosis is a condition where the lining of your uterus (endometrium) grows in other places like your ovaries, vagina or fallopian tubes. It typically causes pelvic pain or severe menstrual cramps. People with PCOS have irregular periods, unpredictable ovulation and other physical side effects due to excess male hormones.
Symptoms and Causes of Endometriosis
Risk factors of polycystic ovary syndrome
You may be more likely to have PCOS if your mother or sister has it. You may also be more likely to have it if you have insulin resistance or are obese.
Complications of polycystic ovary syndrome
Complications of PCOS can include:
- Infertility
- Gestational diabetes or pregnancy-induced high blood pressure
- Miscarriage or premature birth
- Nonalcoholic steatohepatitis. A severe liver inflammation caused by fat buildup in the liver
- Metabolic syndrome. A cluster of conditions including high blood pressure, high blood sugar, and unhealthy cholesterol or triglyceride levels that significantly increase your risk of heart and blood vessel (cardiovascular) disease
- Type 2 diabetes or prediabetes
- Sleep apnea
- Depression, anxiety and eating disorders
- Cancer of the uterine lining (endometrial cancer)
Obesity commonly occurs with PCOS and can worsen complications of the disorder.
Risk factors and Complications of Uterine Fibroids
Polycystic ovary syndrome and miscarriage
Having PCOS may increase your risk for certain pregnancy complications, although most women and people AFAB with PCOS are able to successfully carry a pregnancy. Other complications of PCOS related to pregnancy include increased risk of:
- Gestational diabetes, preeclampsia and high blood pressure.
- Preterm birth (birth before 37 weeks of pregnancy) or C-section delivery due to obesity, diabetes or high blood pressure.
Women with PCOS are more likely to develop certain serious health problems. These include type 2 diabetes, high blood pressure, problems with the heart and blood vessels, and uterine cancer. Women with PCOS often have problems with their ability to get pregnant (fertility).
Prevention of polycystic ovary syndrome
There’s no proven way to prevent PCOS, but you can take small steps to reduce your symptoms. For example, eating nutritious foods, exercising regularly and managing a healthy weight for your body can help you avoid the effects of PCOS.
Diagnosis of polycystic ovary syndrome
Typically, healthcare providers diagnose PCOS if you have at least two of the three symptoms:
- Irregular or missed periods. Some people with PCOS have very heavy bleeding when they do have a period.
- Signs of excess androgens such as acne or excessive hair growth. Or a blood test confirming high androgen levels.
- Enlarged ovaries or polycystic appearance of ovaries on ultrasound. Many people don’t develop cysts.
There’s no single test to specifically diagnose polycystic ovary syndrome (PCOS). Your health care provider is likely to start with a discussion of your symptoms, medications and any other medical conditions. Your provider also may ask about your menstrual periods and any weight changes. A physical exam includes checking for signs of excess hair growth, insulin resistance and acne. Your health care provider might then recommend:
- Pelvic exam. During a pelvic exam, your provider can check your reproductive organs for masses, growths or other changes.
- Blood tests. Blood tests can measure hormone levels. This testing can exclude possible causes of menstrual problems or androgen excess that mimic PCOS. You might have other blood testing, such as fasting cholesterol and triglyceride levels. A glucose tolerance test can measure your body’s response to sugar (glucose).
- Ultrasound. An ultrasound can check the appearance of your ovaries and the thickness of the lining of your uterus. A wandlike device (transducer) is placed in your vagina. The transducer emits sound waves that are translated into images on a computer screen.
If you have a diagnosis of PCOS, your provider might recommend more tests for complications. These tests can include:
- Regular checks of blood pressure, glucose tolerance, and cholesterol and triglyceride levels
- Screening for depression and anxiety
- Screening for obstructive sleep apnea
Prevention and Diagnosis of Ectopic Pregnancy
Treatment of polycystic ovary syndrome
Treatment for PCOS usually starts with lifestyle changes like weight loss, diet, and exercise.
Losing just 5 to 10 percent of your body weight can help regulate your menstrual cycle and improve PCOS symptoms According to The American College of Obstetrician and Gynecologist and National Library of Medicine. Weight loss can also:
- improve cholesterol levels
- lower insulin
- reduce heart disease and diabetes risks
Any diet that helps you lose weight can help your condition. However, some diets may have advantages over others.
Studies comparing diets for PCOS have found that low carbohydrate diets are effective for both weight loss and lowering insulin levels.
A low glycemic index (low GI) diet that gets most carbohydrates from fruits, vegetables, and whole grains helps regulate the menstrual cycle better than a regular weight loss diet. According to Oxford Academic.
A few studies have found that 30 minutes of moderate-intensity exercise at least 3 days a week can help women with PCOS lose weight. Losing weight with exercise also improves ovulation and insulin levels.
Exercise is even more beneficial when combined with a healthy diet. Diet plus exercise helps you lose more weight than either intervention alone, and it lowers your risks for diabetes and heart disease.
There is some evidence that acupuncture can help with improving PCOS, but more research is needed. Learn more here: PubMed Central .
PCOS treatment starts with lifestyle changes like diet and exercise. Losing just 5 to 10 percent of your body weight if you’re overweight can help improve your symptoms.
To regulate your periods, your health care provider might recommend:
- Combination birth control pills. Pills that contain both estrogen and progestin decrease androgen production and regulate estrogen. Regulating your hormones can lower your risk of endometrial cancer and correct irregular bleeding, excess hair growth and acne.
- Progestin therapy. Taking progestin for 10 to 14 days every 1 to 2 months can regulate your periods and protect against endometrial cancer. This progestin therapy doesn’t improve androgen levels and won’t prevent pregnancy. The progestin-only minipill or progestin-containing intrauterine device is a better choice if you also wish to avoid pregnancy.
To help you ovulate so that you can become pregnant, your health care provider might recommend:
- Clomiphene. This oral anti-estrogen medication is taken during the first part of your menstrual cycle.
- Letrozole (Femara). This breast cancer treatment can work to stimulate the ovaries.
- Metformin. This medicine for type 2 diabetes that you take by mouth improves insulin resistance and lowers insulin levels. If you don’t become pregnant using clomiphene, your provider might recommend adding metformin to help you ovulate. If you have prediabetes, metformin can slow the progression to type 2 diabetes and help with weight loss.
- Gonadotropins. These hormone medications are given by injection.
If needed, talk with your health care provider about procedures that may help you become pregnant. For example, in vitro fertilization may be an option.
To reduce excessive hair growth or improve acne, your health care provider might recommend:
- Birth control pills. These pills decrease androgen production that can cause excessive hair growth and acne.
- Spironolactone (Aldactone). This medication blocks the effects of androgen on the skin, including excessive hair growth and acne. Spironolactone can cause birth defects, so effective birth control is needed while taking this medication. This medication isn’t recommended if you’re pregnant or planning to become pregnant.
- Eflornithine (Vaniqa). This cream can slow facial hair growth.
- Hair removal. Electrolysis and laser hair removal are two options for removing hair. Electrolysis uses a tiny needle inserted into each hair follicle. The needle sends out a pulse of electric current. The current damages and then destroys the follicle. Laser hair removal is a medical procedure that uses a concentrated beam of light to remove unwanted hair. You might need multiple treatments of electrolysis or laser hair removal. Shaving, plucking or using creams that dissolve unwanted hair may be other options. But these are temporary, and hair may thicken when it grows back.
- Acne treatments. Medications, including pills and topical creams or gels, may help improve acne. Talk to your health care provider about options.
Surgery / Medical Procedure
- Surgery: A surgical procedure can help restore ovulation by removing tissue in your ovaries that produces androgen hormones. With newer medications available, surgeons rarely perform this procedure.
- In vitro fertilization (IVF): This is an option for people with PCOS when medication doesn’t help with ovulation. Your provider fertilizes your egg with your partner’s sperm in a lab before transferring it to your uterus.
Birth control pills and the diabetes drug metformin can help bring back a normal menstrual cycle. Clomiphene and surgery improve fertility in women with PCOS. Hair removal medications can help women remove unwanted hair.
Diagnosis and Treatment of Abnormal Uterine Bleeding
Polycystic ovary syndrome and pregnancy
PCOS interrupts the normal menstrual cycle and makes it harder to get pregnant. Between 70 and 80 percent of women with PCOS have fertility problems. According to National Center For Biotechnology Information.
This condition can also increase the risk for pregnancy complications.
Women with PCOS are twice as likely as women without the condition to deliver their baby prematurely. They’re also at greater risk for miscarriage, high blood pressure, and gestational diabetes.
However, women with PCOS can get pregnant using fertility treatments that improve ovulation. Losing weight and lowering blood sugar levels can improve your chances of having a healthy pregnancy.
- List of Common Diseases & Medical Disorders
- Buy Complete Premium Anatomy Notes (PDFs)
- Medmichihealthcare New posts
- Read All causes of disease short notes
- Read All diagnosis of disease short notes
- Read All treatment of disease short notes
- Subscribe Medmichihealthcare YouTube channel
Discover more from Medmichihealthcare
Subscribe to get the latest posts sent to your email.