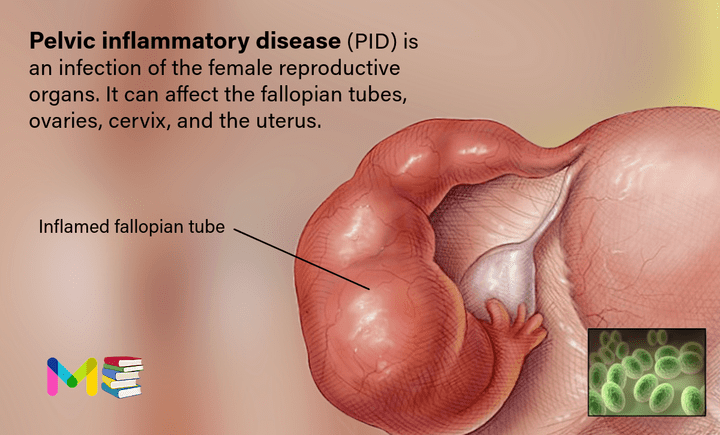
Pelvic inflammatory disease (PID) is an infection of the female reproductive organs. It can affect the fallopian tubes, ovaries, cervix, and uterus.
Pelvic inflammatory disease affects women and people assigned female at birth (AFAB) and occurs most frequently in women between 15 and 25 years old. It mostly occurs when sexually transmitted bacteria spread from your vagina to other reproductive organs.
Several different types of bacteria can cause PID, including the same bacteria that cause the sexually transmitted infections (STIs) gonorrhea and chlamydia. What commonly occurs is that bacteria first enter the vagina and cause an infection. As time passes, this infection can move into the pelvis area or pelvic organs. The pelvis is in the lower abdomen and includes the fallopian tubes, ovaries, cervix, and the uterus.
When you have PID, you may feel pain in your lower abdomen (belly) or pelvis. You may also have unusual discharge (leaking) from your vagina. Untreated PID can cause scar tissue and pockets of infected fluid (abscesses) to develop in the reproductive tract, which can cause permanent damage to your reproductive organs and prevent you from getting pregnant. Getting tested and treated for STIs is the best way to prevent Pelvic inflammatory disease.
Table of Contents
Key points about pelvic inflammatory disease
- Pelvic inflammatory disease (PID) is an infection of a woman’s reproductive tract. It can affect the uterus, fallopian tubes, and/or the ovaries.
- Left untreated, chronic infection and infertility can develop.
- It is caused by bacteria, often the same type of bacteria that causes STDs.
- Sexually active women under age 25, and those of childbearing age are at the greatest risk of getting PID from an STD.
- PID can cause pelvic pain, abdominal tenderness, vaginal discharge, fever, chills, and pain during urination and sex.
- Treatment includes antibiotics, especially if you have a STD.
Key points about polycystic ovary syndrome (PCOS)
Symptoms of pelvic inflammatory disease
The signs and symptoms of pelvic inflammatory disease might be mild and difficult to recognize. Some women with pelvic inflammatory disease don’t have symptoms. For the women who do have symptoms, these can include:
- pain in the lower abdomen (the most common symptom)
- pain in the upper abdomen
- fever
- painful sex
- painful urination
- irregular bleeding
- increased or foul-smelling vaginal discharge
- tiredness
Pelvic inflammatory disease can cause mild or moderate pain. However, some women have severe pain and symptoms, such as:
- sharp pain in the abdomen
- vomiting
- fainting
- a high fever (greater than 101°F)
If you have severe symptoms, call your doctor immediately or go to the emergency room. The infection may have spread to your bloodstream or other parts of your body. This can be life-threatening.
Vaginal discharge with an odor, painful urination or bleeding between periods can also be symptoms of a sexually transmitted infection (STI). If these signs and symptoms occur, stop having sex and see your provider soon. Prompt treatment of an sexually transmitted infection (STI) can help prevent PID.
Read: Symptoms and Causes of Uterine Fibroids
Causes of pelvic inflammatory disease
Bacteria entering your reproductive tract causes pelvic inflammatory disease. These bacteria are passed from your vagina, through your cervix and up into your uterus, fallopian tubes and ovaries. Normally, when bacteria enter your vagina, your cervix keeps them from spreading deeper to other reproductive organs. However, any type of infection can disrupt your cervix, preventing it from doing its job.
Many types of bacteria can cause PID, but the two most common infections that cause PID are gonorrhea and chlamydia. You get both of these infections through unprotected sex. These two STIs cause about 90% of all PID cases.
It can take anywhere from a few days to a few weeks to develop PID if untreated gonorrhea or chlamydia is the cause. If you get PID from something else, it may take several months to develop it.
Less commonly, PID happens when normal bacteria gets into your reproductive organs. This can happen after:
- Childbirth.
- Pelvic surgery.
- Miscarriage.
- Getting an intrauterine device (IUD). The risk is highest in the few weeks after your provider inserts an IUD.
Read: Causes and Risk Factors of Endometriosis
Risk factors of pelvic inflammatory disease
You’re at higher risk for pelvic inflammatory disease if you:
- Have a sexually transmitted infection (STI), especially gonorrhea or chlamydia.
- Have many sexual partners or have a partner who has had multiple partners.
- Have had PID in the past.
- Are sexually active and younger than 25.
- Have had tubal ligation or other pelvic surgery.
- Douching regularly, which upsets the balance of good versus harmful bacteria in the vagina and might mask symptoms
There is a small increased risk of PID after the insertion of an intrauterine device (IUD). This risk is generally confined to the first three weeks after insertion.
Read: Risk Factors and Complications of Adenomyosis
Complications of pelvic inflammatory disease
Untreated pelvic inflammatory disease might cause scar tissue and pockets of infected fluid (abscesses) to develop in the reproductive tract. These can cause permanent damage to the reproductive organs, and lead to several problems including:
- Chronic pelvic pain: Long-lasting pelvic pain is the most common complication. One study estimates about 20% of people develop chronic pelvic pain. Scarring in your fallopian tubes and other pelvic organs can cause pain during intercourse and ovulation.
- Ectopic pregnancy: Scarring can prevent a fertilized egg from moving into your uterus. This can cause it to implant inside your fallopian tubes instead. The rate of ectopic pregnancy in people with PID is much higher than in people without PID. Ectopic pregnancies can cause massive, life-threatening bleeding and require emergency medical attention.
- Infertility: Up to 10% of people with PID lose the ability to get pregnant because scar tissue blocks their fallopian tubes and prevents them from releasing an egg. The more times you’ve had PID, the greater your risk of infertility.
- Tubo-ovarian abscess (TOA): PID might cause an abscess (a collection of pus) to form in your reproductive tract. Most commonly, abscesses affect the fallopian tubes and ovaries, but they can also develop in the uterus or in other pelvic organs. If an abscess is left untreated, you could develop a life-threatening infection.
Read: Complications and Prevention of Low Amniotic Fluid (Oligohyramnios)
Prevention of pelvic inflammatory disease
Sometimes, PID isn’t due to a sexually transmitted infection. It can come from normal vaginal bacteria traveling to your reproductive organs. Avoiding douching may lower the risk.
Most of the time, though, PID happens because of unprotected sex. Take steps to practice safe sex. Ways to protect yourself from sexually transmitted infections (STIs) that can cause PID include:
- Limiting sexual partners: Your risk increases if you have multiple partners.
- Choosing barrier methods of birth control: These types of birth control include condoms and diaphragms. Combine a barrier method with spermicide, even if you take birth control pills.
- Seeking treatment if you notice symptoms: If you notice signs of PID or other STIs, get treatment right away. Symptoms include unusual vaginal discharge, pelvic pain or bleeding between periods.
- Getting regular checkups: Have regular gynecological exams and screenings. Often, providers can identify and treat cervical infections before they spread to reproductive organs.
- Request that your partner be tested. If you have pelvic inflammatory disease or an STI, advise your partner to be tested and treated. This can prevent the spread of STIs and possible recurrence of PID.
- Don’t douche. Douching upsets the balance of bacteria in your vagina.
- Wiping from front to back after using the bathroom. This can help to stop bacteria from entering your vagina
If you’re sexually active, talk to your healthcare provider about yearly testing for sexually transmitted infections. Providers often recommend testing for chlamydia and gonorrhea to help keep you safe. Also, before having sex with a new partner, it’s a good idea for both of you to get tested for STIs.
Read: Prevention and Diagnosis of Abnormal Uterine Bleeding
Diagnosis of pelvic inflammatory disease
If you feel symptoms of PID, see your healthcare provider right away. The sooner you get care, the greater your chances of successful treatment. There isn’t one specific test for PID. Usually, your healthcare provider can diagnose PID through:
- Medical history and physical examination. Asking about your medical history, including your general health, sexual activity and symptoms.
- Pelvic exam. To examine your reproductive organs and feel for tenderness or abscesses (collections of pus).
- Vaginal culture. To test your vaginal discharge for certain bacteria.
- Urine test. To check your urine for signs of blood, cancer, and other diseases
After collecting samples, your doctor sends these samples to a laboratory. Other tests to diagnose pelvic inflammatory disease include:
- Blood tests. These test may be used to test for pregnancy, human immunodeficiency virus (HIV) or other sexually transmitted infections, or to measure white blood cell counts or other markers of infection or inflammation.
- Ultrasound. To get clearer images of your reproductive system. This is an imaging test that uses sound waves to create pictures of your internal organs.
If your doctor determines that you have pelvic inflammatory disease, they may run more tests and check your pelvic area for damage. PID can cause scarring on your fallopian tubes and permanent damage to your reproductive organs.
Additional tests to diagnose PID include:
- Endometrial biopsy. In this outpatient procedure a doctor removes and examines a small sample from the lining of your uterus.
- Laparoscopy. A laparoscopy is an outpatient procedure where a doctor inserts a flexible instrument through an incision in your abdomen and takes pictures of your pelvic organs.
- Pap test. For this test, cells are taken from the cervix and checked under a microscope. It’s used to find cancer, infection, or inflammation.
- Culdocentesis. For this test, a needle is inserted into the pelvic cavity through the vaginal wall to get a sample of pus.
Treatment of pelvic inflammatory disease
Your health care provider will figure out the best treatment based on:
- How old you are
- Your overall health and medical history
- How sick you are
- How well you can handle specific medications, procedures, or therapies
- How long the condition is expected to last
- Your opinion or preference
Prompt treatment with medicine can get rid of the infection that causes pelvic inflammatory disease. But there’s no way to reverse any scarring or damage to the reproductive tract that pelvic inflammatory disease (PID) might have caused. Treatment for PID most often includes:
- Antibiotics. Your health care provider will prescribe a combination of antibiotics to start immediately. After receiving your lab test results, your provider might adjust your prescription to better match what’s causing the infection. You’ll likely follow up with your provider after three days to make sure the treatment is working. Be sure to take all of your medication, even if you start to feel better after a few days.
- Treatment for your partner. To prevent reinfection with an sexually transmitted infection (STI), your sexual partner or partners should be examined and treated. Infected partners might not have any noticeable symptoms.
- Temporary abstinence. Avoid sexual intercourse until treatment is completed and symptoms have resolved.
- Surgery. Surgery is rarely needed. However, if an abscess ruptures or threatens to rupture, your provider might drain it. You might also need surgery if you don’t respond to antibiotic treatment or have a questionable diagnosis, such as when one or more of the signs or symptoms of PID are absent.
If you’re pregnant, seriously ill, have a suspected abscess or haven’t responded to oral medications, you might need hospitalization. You might receive intravenous (IV) antibiotics, followed by antibiotics you take by mouth.
Pelvic inflammatory disease is a very treatable condition and most women make a full recovery. However, according to the Centers for Disease Control and Prevention, about 1 in 8 women with a history of PID will have difficulty getting pregnant. Pregnancy is still possible for most women.
Read: Diagnosis and Treatment of Preeclampsia
- List of Common Diseases & Medical Disorders
- Buy Complete Premium Anatomy Notes (PDFs)
- Medmichihealthcare New posts
- Read All causes of disease short notes
- Read All diagnosis of disease short notes
- Read All treatment of disease short notes
- Subscribe Medmichihealthcare YouTube channel
Discover more from Medmichihealthcare
Subscribe to get the latest posts sent to your email.