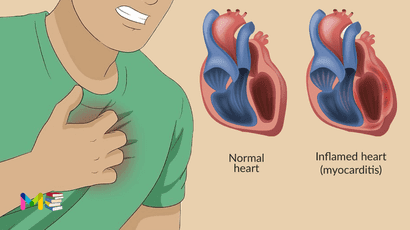
Myocarditis is an inflammation of the heart muscle (myocardium). This can weaken your heart muscle, making it more difficult for your heart to pump. This rare condition can affect people quickly or slowly over time.
It can cause chest pain, shortness of breath, and rapid or irregular heart rhythms (arrhythmias).
Severe myocarditis weakens the heart so that the rest of the body doesn’t get enough blood. Clots can form in the heart, leading to a stroke or heart attack. Treatment for myocarditis may include medications, procedures or surgeries.
Study estimate there are about 1.5 million cases of myocarditis in the world each year. This works out to 10 to 20 people affected out of every 100,000 people.
Table of Contents
Symptoms of myocarditis
Some people with early myocarditis don’t have symptoms. Others may have mild symptoms, which include:
- fatigue
- chest pain
- heart palpitations
- shortness of breath, both at rest and with exertion
- swelling in your legs or feet
- weakness
- lightheadedness or fainting
Because myocarditis is often caused by a viral infection, you may also experience flu-like symptoms prior to the onset of myocarditis symptoms. This can include symptoms such as:
- body aches
- fever
- fatigue
Symptoms of myocarditis in children include:
- Chest pain
- Breathing difficulties
- Fever
- Rapid breathing
- Rapid or irregular heart rhythms (arrhythmias)
- Fainting
You can also read about symptoms and causes of heart failure.
Causes of myocarditis
Mostly, the causes of myocarditis are viral infection. These include:
- Flu.
- Herpes virus six.
- Adenovirus.
- Coxsackie virus.
- SARS-CoV-2 (COVID-19).
- Parvovirus B19.
Some other causes may include:
- Bacteria.
- Fungi (rarely).
- Chagas disease.
- Rheumatic fever.
- Things you’re exposed to, such as radiation or heavy metals.
- Autoimmune diseases like rheumatoid arthritis or lupus.
Causes from some medications side effects, such as:
- Antidepressants.
- Medicines for your heart.
- Medicines for seizures.
- Antibiotics.
- Medicines for weight loss.
- Diuretics.
- Medicines for psychiatric problems.
- Benzodiazepines.
You can also read about symptoms and risk factors of asthma.
Risk factors myocarditis
You’re more likely to get myocarditis if:
- You take too much of alcohol than the limit your healthcare provider gives you.
- Your body doesn’t react well to inflammation. Although you don’t inherit myocarditis, your genes influence how your body handles inflammation and how likely you are to get myocarditis.
Medical treatments that can increase your risk of myocarditis:
- Radiation.
- Dialysis.
- Treatments for heart problems.
- Having a central venous line.
- Implanted heart devices.
Having some of the following medical conditions and problems can also put you at risk of myocarditis:
- HIV/AIDS.
- Diabetes.
- Skin injuries or infections.
- Cancer treated with certain medicines.
- A chest injury.
- End-stage kidney disease.
- Eating disorders.
You can also read about risk factors and complications of high blood pressure.
Complications of myocarditis
Usually, myocarditis goes away without permanent complications. However, severe myocarditis can permanently damage the heart muscle.
Potential complications of myocarditis may include:
- Rapid or irregular heart rhythms (arrhythmias). Damage to the heart muscle can change how the heart beats. Certain arrhythmias increase the risk of stroke.
- Heart attack or stroke. If the heart muscle is injured and can’t pump blood, the blood that collects in the heart can form clots. A heart attack can occur if a clot blocks one of the heart (coronary) arteries. A stroke can occur if a blood clot in the heart travels to an artery leading to the brain.
- Heart failure. Untreated, myocarditis can damage the heart muscle so that it can’t pump blood well. In severe cases, myocarditis-related heart failure may require a ventricular assist device or a heart transplant.
- Sudden cardiac death. Certain serious arrhythmias can cause the heart to stop beating (sudden cardiac arrest). It’s deadly if not treated immediately (sudden cardiac death).
Prevention of myocarditis
It’s not possible to completely prevent myocarditis. However, taking steps to avoid infections can help lower your risk of developing myocarditis. Steps you can take include:
1 washing your hands regularly, particularly in the following scenarios:
- after coughing, sneezing, or blowing your nose
- after using the bathroom or changing a diaper
- after being out in public
- before and after handling or preparing food
- before eating
2 making sure you’re up to date with your vaccinations.
3 avoiding close contact with people who are sick.
4 practicing safer sex behaviors, such as:
- using a condom or other barrier method during sex
- getting tested regularly for sexually transmitted infections (STIs)
- discussing STI history with new sexual partners prior to having sex
5 avoiding ticks, which can cause Lyme disease, when you’re outdoors
Diagnosis of myocarditis
Early diagnosis of myocarditis is important to preventing long-term heart damage. To diagnose myocarditis, a health care provider will typically examine you and listen to your heart with a stethoscope. Your provider will also ask:
- whether you’ve had an infection recently
- if you’ve been previously diagnosed with myocarditis
- questions about your symptoms
The following tests are used to diagnose myocarditis:
- Blood tests. Blood tests use a sample of blood from a vein in your arm to check for signs of infection or inflammation.
- Echocardiogram. An echocardiogram creates an ultrasound image of the heart and can help detect structural or functional issues in the heart and adjacent blood vessels.
- Electrocardiogram (ECG). An ECG measures the electrical activity in your heart and can be used to detect abnormal heart rates and rhythms that may indicate damaged heart muscle.
- Chest X-ray. A chest X-ray can show chest anatomy and potential signs of heart failure.
- Heart CT scan. A heart CT scan uses multiple X-ray images to create a cross-sectional, detailed image of your heart.
- Myocardial biopsy. With a myocardial biopsy, a small sample of heart muscle tissue is collected during a heart catheterization. This allows your doctor to examine the sample for signs of myocarditis.
- Heart MRI. A heart MRI can detect signs of inflammation in your heart muscle; it can also allow your doctor to evaluate your heart’s size and shape.
You can also read about diagnosis and treatment of stroke.
Treatment of myocarditis
If you have a mild case, it may go away on its own. Myocarditis treatment focuses on the cause and the symptoms, such as heart failure.
Medication treatment
People with mild myocarditis may only need rest and medication. Medications to treat myocarditis may include:
- Heart medications. If myocarditis is causing severe heart failure or irregular heartbeats, drugs may be given to reduce the risk of blood clots in the heart.For a weak heart, medications can help remove extra fluid from the body and reduce the strain on the heart. Some types of medications that may be given are diuretics, beta blockers, angiotensin-converting enzyme (ACE) inhibitors or angiotensin II receptor blockers (ARBs).
- Corticosteroids. These medicines suppress the immune system. They may be used to treat some rare types of viral myocarditis, such as giant cell and eosinophilic myocarditis.
- IV medications. Medications given through an IV are used to quickly improve the heart’s ability to pump.
- Medications to treat underlying conditions. Sometimes another health condition, such as lupus, causes myocarditis. Treating the underlying condition may help reduce heart muscle inflammation.
Some people with myocarditis may need medications for just a few months and then recover completely. Others may have long-term, permanent heart damage that needs lifelong medication. It’s important to have regular health checkups after a diagnosis of myocarditis to check for possible complications.
Medical surgeries and procedures
If you have severe myocarditis, you will need aggressive treatment, which might include:
- Intra-aortic balloon pump. This device helps increase blood flow and lower the strain on the heart. The heart doctor (cardiologist) inserts a thin tube (catheter) into a blood vessel in the leg and guides it to the heart. A balloon attached to the end of the catheter inflates and deflates in the main artery leading out to the body from the heart (aorta).
- Ventricular assist device (VAD). A VADhelps pump blood from the lower chambers of the heart (the ventricles) to the rest of the body. It’s a treatment for a weakened heart or heart failure. A VADmay be used to help the heart work while waiting for other treatments, such as a heart transplant.
- Extracorporeal membrane oxygenation (ECMO). An ECMO machine works like the lungs.It removes carbon dioxide and adds oxygen to the blood. If you have severe heart failure, this device can send oxygen to your body. During ECMO, blood is removed from the body, passed through the machine and then returned to the body.ECMO may be used to help the heart to recover or while waiting for other treatments, such as a heart transplant.
- Heart transplant. An urgent heart transplant may be needed for those who have very severe myocarditis.
If you have myocarditis, you should avoid competitive sports for at least 3 to 6 months. Following a healthy lifestyle is an important part of myocarditis treatment and recovery.
- List of Common Diseases & Medical Disorders
- Buy Complete Premium Anatomy Notes (PDFs)
- Medmichihealthcare New posts
- Read All causes of disease short notes
- Read All diagnosis of disease short notes
- Read All treatment of disease short notes
- Subscribe Medmichihealthcare YouTube channel
Discover more from Medmichihealthcare
Subscribe to get the latest posts sent to your email.