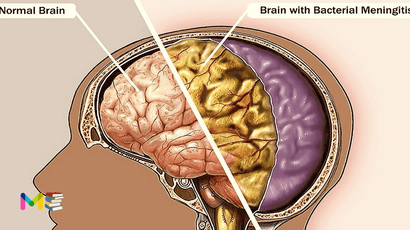
Meningitis is the infection and inflammation of the fluid and membranes (meninges) surrounding the brain and spinal cord. Bacteria, viruses, fungi, parasites and non-infectious conditions are the causes of meningitis.
Inflammation of the meninges typically triggers symptoms such as headache, fever and a stiff neck. Most cases of meningitis are caused by a viral infection. But bacteria, parasites and fungi also can cause it. Some cases of meningitis improve without treatment in a few weeks. Others can cause death and require emergency antibiotic treatment.
Table of Contents
The meninges
Meninges are what protects your brain and spinal cord from injury and provide support and structure. They contain nerves, blood vessels and protective fluid (cerebrospinal fluid).
Bacteria infections, viral infections and non-infections disease are what causes meningitis. Non-infectious disease like cancer or head injuries, can cause meningitis.
Spinal and aseptic meningitis
Spinal meningitis is other name for meningitis, which mean, an inflammation of the meninges surrounding your brain and spinal cord.
While Aseptic meningitis is any case of meningitis where the fluid around your brain and spine (CSF) tests negative for bacteria infection. This means either the bacteria causing meningitis is difficult to grow or that your case of meningitis isn’t caused by bacteria. The most common cause of aseptic meningitis is a viral infection.
Symptoms of meningitis
Early signs of meningitis can be similar to the flu. Symptoms can develop over several hours or over few days. The possible signs and symptoms in anyone older than the age of 2 years include:
- Severe headache.
- Sudden high fever.
- Stiff neck.
- Nausea or vomiting.
- Confusion or trouble concentrating.
- Seizures.
- Sleepiness or trouble waking.
- Sensitivity to light.
- Skin rash in some cases, such as in meningococcal meningitis.
- No appetite or thirst.
Signs in newborn and infants include:
- Constant crying.
- High fever.
- Being very sleepy or irritable.
- Trouble waking from sleep.
- Being inactive or sluggish.
- Not waking to eat.
- Poor feeding.
- Vomiting.
- Stiffness in the body and neck.
- A bulge in the soft spot on top of the baby’s head.
Baby with this condition may be hard to comfort. They can even cry harder when held.
You should Seek medical emergency immediately if you or someone in your family has the following symptoms, such as:
- Severe headache that doesn’t go away.
- Fever.
- Confusion.
- Stiff neck.
- Vomiting.
The bacterial meningitis is serious and can cause death within days without fast approach with antibiotic treatment. Delaying the treatment also increases the risk of permanent damaged brain.
It’s also important to talk to your doctor if you’ve been exposed to someone with meningitis. That may include a family member or someone you live or work with. You may need to take medicines to prevent getting infected.
Chronic meningitis is when your symptoms last longer than 4 weeks. The symptoms of chronic meningitis are similar to other forms of acute meningitis, but can sometimes develop slower.
You can also read about symptoms and types of migraine headaches.
Types of meningitis
Viral and bacterial meningitis are the most common types. There are several other forms of meningitis. This include cryptococcal, which is caused by a fungal infection, and carcinomatous, which is cancer-related. The whole forms of meningitis include:
- Viral meningitis.
- Bacterial meningitis.
- Fungal meningitis.
- Parasitic meningitis. Meningitis caused by certain parasites is called eosinophilic meningitis or eosinophilic meningoencephalitis (EM).
- Primary Amebic Meningitis. Meningitis can be caused by the ameba Naegleria fowleri.
- Drug-induced aseptic meningitis. Rarely, certain medications cause drug-induced aseptic meningitis (DIAM). Non-steroidal anti-inflammatory drugs (NSAIDS) and antibiotics are the most common causes of DIAM.
- Acute meningitis. Bacterial meningitis is often acute, meaning that symptoms are severe and come on suddenly.
- Chronic meningitis. When meningitis has lasted a month or more, it’s called chronic meningitis.
Causes of meningitis
Infectious diseases from outside your body and non-infectious conditions cause meningitis.
Infectious causes include bacteria, viruses, fungi, parasites and the ameba Naegleria fowleri. While Non-infectious causes include diseases, certain medications and other conditions. Causes depending on types include:
Bacterial meningitis:
- Group B Streptococcus.
- Streptococcus pneumonia.
- Neisseria meningitides.
- Haemophilus influenza.
- Listeria monocytogenes.
- Mycobacterium tuberculosis.
- E. coli.
Viral meningitis:
- Mumps.
- Non-polio enteroviruses.
- Herpesviruses (including those that cause mononucleosis, chickenpox and shingles).
- Measles.
- Influenza.
- Lymphocytic choriomeningitis virus.
- Arboviruses, such as West Nile virus.
Parasitic meningitis:
- Baylisascaris procyonis.
- Gnathostoma spinigerum.
- Angiostrongylus cantonensis.
Fungal meningitis:
- Coccidioides.
Amebic meningitis:
- Naegleria fowleri causes amebic meningitis.
Non-infectious meningitis
- Certain medications, like NSAIDs and antibiotics.
- Head injuries.
- Brain surgery.
- Systemic lupus erythematosus (lupus).
Swelling of the meninges isn’t contagious, but some of the causes of it are. Most bacterial and viral causes of meningitis can be spread from person to person. You can’t catch other causes of meningitis from another person.
You can also read about causes and risk factors of heart attack.
Risk factors of meningitis
The following are some of the risk factors:
- Compromised immunity. People with an immune deficiency are more vulnerable to infections. This includes the infections that cause meningitis. Certain disorders and treatments can weaken your immune system. These include HIV/AIDS, autoimmune disorders, chemotherapy, organ or bone marrow transplants, cancer, immunosuppressive medication. The cryptococcal meningitis, which is caused by a fungus, is the most common form of meningitis in people with HIV.
- Community areas: Meningitis can be easily spread when people live in close quarters. Being in small spaces increases the chance of exposure. Examples include college dormitories, barracks, boarding schools, daycare centers, assisted living facilities.
- Pregnancy: Pregnant women have an increased risk of listeriosis, which is an infection caused by the Listeria bacteria. Infection can spread to the unborn child.
- Your age: All ages are at risk for meningitis. However, certain age groups have a higher risk. Children under the age of 5 are at increased risk of viral meningitis. Infants are at higher risk of bacterial meningitis. Older adults can also be at risk for certain infections that can lead to meningitis.
- Exposure to animals: Farm workers and others who work with animals have an increased risk of infection with Listeria.
- Not vaccinated. Risk rises for anyone who hasn’t completed the recommended childhood or adult vaccination schedule.
Complications of meningitis
Meningitis complications can be severe, especially the bacteria one. The longer you or your child has the disease without treatment, the greater the risk of seizures and permanent neurological damage could happen. This complications include:
- Seizures.
- Hearing loss.
- Memory problems.
- Learning disabilities.
- Brain damage.
- Trouble walking.
- Kidney failure.
- Shock.
- Death.
With proper treatment and early approach, even people with severe condition can have good recovery and live a healthy life.
Prevention of meningitis
The best steps to take to reduce your risk of meningitis is to take simple precautions to protect yourself from the infectious diseases that most often cause it. Getting vaccinated, practicing safe food handling and washing your hands are a few ways to reduce your risk of getting infectious diseases. Your healthcare provider might also recommend using antibiotics such as prophylactic to prevent infections in specific situations.
Other preventive measures include:
- Disinfect frequently touched surfaces.
- Wash your hands frequently with soap and water. Thorough hand-washing is particularly important after using the bathroom, before and after preparing a meal or eating, after contact with poop (animal or human) and after gardening or working with sand or dirt.
- Cover your mouth and nose when you cough or sneeze.
- Avoid contact with others when either of you are sick with a contagious disease. If you can’t avoid others, wearing a mask may help prevent the spread of disease. Don’t share personal items (like drinking glasses) with other people.
- Don’t swim in or drink water that could be contaminated. Use distilled or treated water for nasal irrigation.
- Practice safe food prep: Freeze and cook foods to safe temperatures. Peel or thoroughly wash all fruits and vegetables. Wash food preparation surfaces and utensils with soap and water after use.
- Don’t eat undercooked or uncooked meat and seafood.
- Don’t drink unpasteurized milk or eat food made from unpasteurized milk.
- Reduce your risk of bug bites by using bug repellent approved for ticks and mosquitos and covering as much exposed skin as you can when outside. Check for ticks after being in wooded areas or areas with long grass.
- Reduce your risk of fungal infections by wearing a mask in dusty areas like constructions sites and staying inside during dust storms. Take extra precautions if you live in areas where fungal infections are common.
- When traveling, learn how to reduce your risk of infectious diseases that are common in your destination.
- If you’re pregnant, follow your healthcare provider’s recommendations on which foods to avoid. Ask about testing for group B S__treptococcus and how to avoid passing an infection to your baby during birth.
You can also read about complications and prevention of pneumonia.
Diagnosis of meningitis
The diagnosis starts with a health history and physical examinations. Your Age, dorm residence, and daycare center attendance can be important clues. During the physical exam, your doctor will look for the following:
- neck stiffness
- fever
- skin issues
- increased heart rate
- reduced consciousness
Your healthcare provider will also order a lumbar puncture. This test is also called a spinal tap. It allows your doctor to analyze the cerebral spinal fluid, which contains a number of clues regarding an infection. Some of the clues in the cerebral spinal fluid can be glucose, white blood cell count, and red blood cell count. This test can also determine the best antibiotic for treatment.
Other tests to diagnose meningitis include:
- Blood cultures identify bacteria in the blood. Bacteria can travel from the blood to the brain. N. meningitidis and S. pneumonia, among others, can cause both sepsis and meningitis.
- A complete blood count with differential is a general index of health. It checks the number of red and white blood cells in your blood. White blood cells fight infection. The count is usually elevated in meningitis.
- A CT-scan. The scanning of the head may show problems like a brain abscess or or intercranial pressure. Bacteria can spread from the sinuses to the meninges.
- Chest X-rays. This can reveal the presence of pneumonia, tuberculosis, or fungal infections. Meningitis can occur after pneumonia.
- Stool sample. Your doctor may order for a sample of your poop (stool). A lab will test your stool sample for signs of infection.
Treatment of meningitis
Treatment depends on what is causing the infection. Antibiotics are used to treat bacterial meningitis and antifungals are used to treat fungal meningitis. Antivirals can be used to treat some viral causes of meningitis. Non-infectious causes of meningitis are treated by addressing the underlying conditions or injury.
There are no specific treatments for other infectious causes of meningitis. Drugs might be used to reduce inflammation or relieve your signs and symptoms.
Medications and other treatment therapies that can be used to treat this condition include:
- Antivirals for certain cases of viral meningitis, like herpesvirus and influenza.
- Antibiotics for bacterial meningitis.
- Antifungals for fungal meningitis.
- Corticosteroids, like dexamethasone or prednisone, to reduce inflammation.
- IV fluids to keep you hydrated.
- Pain relievers.
You can start to feel better in few days up to a week after starting treatment. The full recovery may take weeks or months.
You can also read about diagnosis and treatment of myocarditis.
Vaccination of meningitis
The following vaccinations can be used in the prevention of meningitis.
- Pneumococcal conjugate vaccine (PCV13 or PCV15). These vaccines also are part of the CDC recommended routine vaccination schedule for children younger than 2 years. Additional doses are recommended for children between the ages of 2 and 5 who are at high risk of pneumococcal disease, including children who have chronic heart or lung disease or cancer.
- Haemophilus influenzae type b vaccine (Hib). The World Health Organization (WHO) and the Centers for Disease Control and Prevention (CDC) recommend this vaccine for children starting at about 2 months of age. The vaccine also is recommended for some adults, including those who have sickle cell disease or AIDS and those who don’t have a spleen.
- Pneumococcal polysaccharide vaccine (PPSV23). Older children and adults who need protection from pneumococcal bacteria may receive this vaccine. The CDC recommends the PPSV23 vaccine for all adults older than 65; for younger adults and children age 2 and older who have weak immune systems or chronic illnesses such as heart disease, diabetes or sickle cell anemia; and for anyone who doesn’t have a spleen.
- Serogroup B meningococcal vaccine (MenB). The CDC recommends this vaccine for adults and children 10 years and older who are at increased risk of meningococcal disease. They include adults and children with sickle cell disease, who have a damaged spleen or who have had their spleen removed. They also include people with the rare immune disorder called complement component deficiency or who take certain medicines. This vaccine may be recommended if you’re in a population that’s having an outbreak of serogroup B meningococcal disease.
- Meningococcal conjugate vaccine (MenACWY). The CDC recommends that a single dose be given to children ages 11 to 12, with a booster shot given at age 16. If the vaccine is first given between ages 13 and 15, the booster is recommended between ages 16 and 18. If the first shot is given at age 16 or older, no booster is necessary.This vaccine also can be given to children between the ages of 2 months and 10 years who are at high risk of bacterial meningitis or who have been exposed to someone with the disease. It’s also used to vaccinate healthy but previously unvaccinated people who have been exposed in outbreaks.
- List of Common Diseases & Medical Disorders
- Buy Complete Premium Anatomy Notes (PDFs)
- Medmichihealthcare New posts
- Read All causes of disease short notes
- Read All diagnosis of disease short notes
- Read All treatment of disease short notes
- Subscribe Medmichihealthcare YouTube channel
Discover more from Medmichihealthcare
Subscribe to get the latest posts sent to your email.