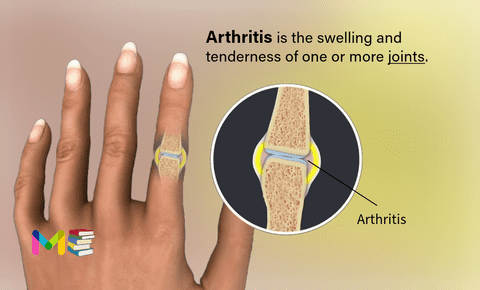
Arthritis is the swelling (inflammation) and tenderness of one or more joints in your body. Joints are places in your body where two bones meet.
Some joints naturally wear down as you age. Lots of people develop arthritis after that normal, lifelong wear and tear. Some types of arthritis happen after injuries that damage a joint. Certain health conditions also cause arthritis.
There are more than 100 different types of arthritis, with different causes and treatment methods.
The main symptoms of arthritis are joint pain and stiffness, which typically worsen with age. The most common types of arthritis are osteoarthritis and rheumatoid arthritis.
The typical age for developing rheumatoid arthritis (RA) is between ages 30 and 50. It can, however, affect children, teens, and younger adults.
Osteoarthritis (OA) commonly develops after the age 50 or 60 years, but there are studies that reveal radiographic evidence of OA occurring in women in their 40s. It also tends to be more prevalent in individuals who are overweight.
Table of Contents
Key points about arthritis
- Arthritis and other rheumatic diseases cause pain, swelling, and limited movement in joints and connective tissues in the body.
- Arthritis and other rheumatic diseases can affect people of all ages. They are more common in women than men.
- Symptoms may include pain, stiffness, swelling, warmth, or redness in 1 or more joints.
- There is no cure for arthritis. The treatment goal is to limit pain and inflammation and preserve joint function.
- Treatment options include medicines, weight reduction, exercise, and surgery.
Common locations of arthritis
Arthritis can affect any joint, but is most common in people’s:
- Hands and wrists.
- Knees.
- Hips.
- Feet and ankles.
- Shoulders.
- Lower back (lumbar spine).
Types of arthritis
There are more than 100 different types of arthritis. Some of the most common types include:
- Osteoarthritis: Wear and tear arthritis.
- Rheumatoid arthritis: Arthritis that happens when your immune system mistakenly damages your joints.
- Gout: Arthritis that causes sharp uric acid crystals to form in your joints.
- Ankylosing spondylitis: Arthritis that affects joints near your lower back.
- Psoriatic arthritis: Arthritis that affects people who have psoriasis.
- Juvenile arthritis: Arthritis in kids and teens younger than 16.
- Scleroderma. This autoimmune disease causes thickening and hardening of the skin and other connective tissue in the body.
Depending on which type of arthritis you have, it can break down the natural tissue in your joint (degeneration) or cause inflammation (swelling). Some types cause inflammation that leads to degeneration.
Symptoms of arthritis
Joint pain, stiffness, and swelling are the most common symptoms of arthritis. Your symptoms may also feel worse in the morning when you get out of bed or upon standing up after you’ve been resting.
Other symptoms of osteoarthritis include:
- limited range of motion that sometimes goes away after movement
- clicking or popping with bending
- muscle weakness around the joint
- instability or buckling of the joint
- bony growths in the fingers
- grating or scraping feeling in the knees
Other symptoms of rheumatoid arthritis include:
- morning stiffness that can last 30 minutes or more
- more than one affected joint
- onset in smaller joints like feet and hands
- same joints on both sides of the body are affected
- fatigue
- low-grade fever
- inflammation of the eyes and mouth
- inflammation of the heart muscle and blood vessels
- low red blood cell count
Where you experience symptoms depends on which type of arthritis you have, and which of your joints it affects.
Some types of arthritis cause symptoms in waves that come and go called flares or flare-ups. Others make your joints feel painful or stiff all the time, or after being physically active.
Types and Symptoms of Sciatica (nerve pain)
Causes of arthritis
Arthritis may be caused by:
- wear and tear of a joint from overuse
- age (OA is most common in adults over age 50)
- injuries
- obesity
- autoimmune disorders
- genes or family history
- muscle weakness
What causes arthritis also varies depending on which type you have:
- Osteoarthritis happens naturally as you age, a lifetime of using your joints can eventually wear down their cartilage cushioning.
- You may develop gout if you have too much uric acid in your blood (hyperuricemia).
- Your immune system can cause arthritis (including rheumatoid arthritis) when it damages your joints by mistake.
- Certain viral infections (including COVID-19) can trigger viral arthritis.
- Sometimes, arthritis happens with no cause or trigger. Providers call this idiopathic arthritis.
Risk factors of arthritis
Some risk factors for arthritis that can’t be avoided or changed include:
- Age. The older you are, the more likely you are to have arthritis.
- Gender. Women are more likely to have arthritis than men.
- Heredity. Some types of arthritis are linked to certain genes.
Risk factors that may be avoided or changed include:
- Weight. Being overweight or obese can damage your knee joints. This can make them more likely to develop osteoarthritis.
- Injury. A joint that has been damaged by an injury is more likely to develop arthritis at some point.
- Infection. Reactive arthritis can affect joints after an infection.
- Your job. Work that involves repeated bending or squatting can lead to knee arthritis.
Causes and Risk Factors Of Diabetes
Complications of arthritis
When left untreated, symptoms of arthritis may worsen and affect your day-to-day life. Below are some of the possible complications associated with this condition:
- Reduced mobility. As arthritis progresses, you may experience less comfortable movement. This can interfere with your daily routine and may keep you from your favorite activities as well as socializing.
- Possible weight gain. This is attributed to decreased movements, as well as discomfort that keeps you from exercising.
- Increased risk of metabolic disorders. Being overweight with an inflammatory condition like arthritis may increase your chances of developing type 2 diabetes, high blood pressure, high cholesterol, and heart disease.
- Inflammation in other areas of your body. If your arthritis is attributed to an autoimmune disease like with RA, the inflammation can spread and affect your skin, eyes, blood vessels, and lungs.
- Risk of falls. According to the Arthritis Foundation, people with OA are more likely to experience falls and possible fractures. This is primarily caused by related muscle weakness, but dizziness from pain medications can also lead to falls.
- Decreased ability to work. The Centers for Disease Control and Prevention (CDC) estimates that about 60 percent of people with arthritis are working age. Arthritis may affect your ability to move around in the workplace or even get from your mode of transportation to your job site.
- Effects on mental health. Arthritis may increase the risk of anxiety and depression due to ongoing pain, inflammation, and social isolation.
Prevention of arthritis
Some forms of arthritis happen naturally or because of health conditions you can’t change, so there’s not always a way to prevent it. However, you can lower your chances of developing arthritis by:
- Avoiding tobacco products.
- Following a diet and exercise plan that’s healthy for you.
- Doing low-impact exercise.
- Always wearing proper protective equipment for any activity that could damage your joints.
Complications And Prevention of Paralysis
Diagnosis of arthritis
Your healthcare provider will take your medical history and give you a physical exam. Tests may also be done. These include blood tests such as:
- Antinuclear antibody (ANA) test. This checks antibody levels in the blood.
- Complete blood count (CBC). This checks if your white blood cell, red blood cell, and platelet levels are normal.
- Creatinine. This test checks for kidney disease.
- Sedimentation rate. This test can find inflammation.
- Hematocrit. This test measures the number of red blood cells.
- RF (rheumatoid factor) and CCP (cyclic citrullinated peptide) antibody tests. These can help diagnose rheumatoid arthritis. They can also assess how severe the disease is.
- White blood cell count. This checks the level of white blood cells in your blood.
- Uric acid. This helps diagnose gout.
Other tests may be done, such as:
- Joint aspiration (arthrocentesis). A small sample of synovial fluid is taken from a joint. It’s tested to see if crystals, bacteria, or viruses are present.
- X-rays or other imaging tests. These can tell how damaged a joint is.
- Urine test. This checks for protein and different kinds of blood cells.
- HLA tissue typing. This looks for genetic markers of ankylosing spondylitis.
- Skin biopsy. Tiny tissue samples are removed and checked under a microscope. This test helps to diagnose a type of arthritis that involves the skin, such as lupus or psoriatic arthritis.
- Muscle biopsy. Tiny tissue samples are removed and checked under a microscope. This test helps to diagnose conditions that affect muscles.
Treatment of arthritis
The main goal of treatment is to reduce the amount of pain you’re experiencing and prevent additional damage to the joints. You’ll learn what works best for you in terms of managing pain. In general, treatment for arthritis involves a combination of:
- medications and supplements
- physical therapy
- occupational therapy
- nutrient-rich diet
- regular exercise
- weight loss, if needed
- heat and cold compresses
- mobility assistance devices, such as canes or walkers
Improving your joint function is also important. Your doctor may prescribe a combination of treatment methods to achieve the best results.
Medications
The medications used to treat arthritis vary depending on the type of arthritis. Commonly used arthritis medications include:
- Analgesics, such as hydrocodone (Vicodin) or acetaminophen (Tylenol), are effective for pain management, but do not help decrease inflammation.
- Nonsteroidal anti-inflammatory drugs (NSAIDs). This can relieve pain and reduce inflammation. Examples include ibuprofen (Advil, Motrin IB, others) and naproxen sodium (Aleve). Stronger NSAIDs can cause stomach irritation and may increase your risk of heart attack or stroke. NSAIDs are also available as creams or gels, which can be rubbed on joints.
- Counterirritants. Some varieties of creams and ointments contain menthol or capsaicin, the ingredient that makes hot peppers spicy. Rubbing these preparations on the skin over your aching joint may interfere with the transmission of pain signals from the joint itself.
- Steroids. Corticosteroid medications, such as prednisone, reduce inflammation and pain and slow joint damage. Corticosteroids may be given as a pill or as an injection into the painful joint. Side effects may include thinning of bones, weight gain and diabetes.
- Menthol or capsaicin creams. These creams block the transmission of pain signals from your joints.
- Immunosuppressants and biologics. Immunosuppressants and biologics are prescribed for moderate to severe inflammatory arthritis like RA.
- Disease-modifying antirheumatic drugs (DMARDs). These drugs can slow the progression of rheumatoid arthritis and save the joints and other tissues from permanent damage. In addition to conventional DMARDs, there are also biologic agents and targeted synthetic DMARDs. Side effects vary but most DMARDs increase your risk of infections.
If you have RA, your doctor may recommend corticosteroids or disease-modifying antirheumatic drugs (DMARDs), which suppress your immune system.
DMARDs and biologics are being prescribed earlier in the course of RA. Methotrexate is now a first-line drug for treatment. There are also many medications to treat OA available over the counter or by prescription.
Therapy
Physical therapy can be helpful for some types of arthritis. Exercises can improve range of motion and strengthen the muscles surrounding joints. In some cases, splints or braces may be warranted.
Surgery
You may need surgery if you have severe arthritis and other treatments don’t work, your healthcare provider may suggest surgery, such as:
- Joint repair. In some instances, joint surfaces can be smoothed or realigned to reduce pain and improve function. These types of procedures can often be performed arthroscopically — through small incisions over the joint.
- Joint replacement. This procedure removes the damaged joint and replaces it with an artificial one. Joints most commonly replaced are hips and knees.
- Joint fusion. This procedure is more often used for smaller joints, such as those in the wrist, ankle and fingers. It removes the ends of the two bones in the joint and then locks those ends together until they heal into one rigid unit.
Alternative medicine and Home remedies
Many people use alternative remedies for arthritis, but there is little reliable evidence to support the use of many of these products. The most promising alternative remedies for arthritis include:
- Acupuncture. This therapy uses fine needles inserted at specific points on the skin to reduce many types of pain, including that caused by some types of arthritis.
- Glucosamine. Although study results have been mixed, some studies have found that glucosamine works no better than placebo. However, glucosamine and the placebo both relieved osteoarthritis pain better than taking nothing, particularly in people who have moderate to severe pain from knee osteoarthritis.
- Chondroitin. Chondroitin may provide modest pain relief from osteoarthritis, although study results are mixed.
- Fish oil. Some preliminary studies have found that fish oil supplements may reduce the symptoms of some types of arthritis. Fish oil can interfere with medications, so check with your doctor first.
- Yoga and tai chi. The slow, stretching movements associated with yoga and tai chi may help improve joint flexibility and range of motion.
- Massage. Light stroking and kneading of muscles may increase blood flow and warm affected joints, temporarily relieving pain. Make sure your massage therapist knows which joints are affected by arthritis.
Diagnosis And Treatment Of Appendicitis
Arthritis can be a pain in the neck (and knees, and hips, and back and any other joint in your body), but try to stay as active as possible. Ask your provider about physical or occupational therapy to help you stay strong, active and confident throughout your daily routine.
- List of Common Diseases & Medical Disorders
- Buy Complete Premium Anatomy Notes (PDFs)
- Medmichihealthcare New posts
- Read All causes of disease short notes
- Read All diagnosis of disease short notes
- Read All treatment of disease short notes
- Subscribe Medmichihealthcare YouTube channel
Discover more from Medmichihealthcare
Subscribe to get the latest posts sent to your email.