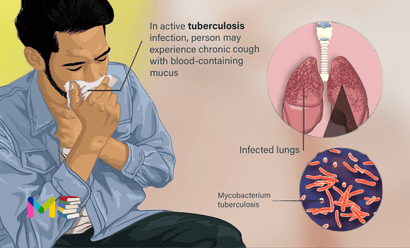
Tuberculosis (TB) is a disease caused by bacteria known as Mycobacterium tuberculosis. This can cause infection in your lungs or other tissues. It commonly affects your lungs, but it can also affect other organs like your spine, brain or kidneys. The word “tuberculosis” comes from a Latin word for “nodule” or something that sticks out.
When the bacterium that causes TB, does not experience symptoms. This condition is known as latent TB. TB can stay dormant for years before developing into active TB disease.
Active TB typically causes many symptoms. While symptoms usually relate to the respiratory system, they could affect other parts of the body, depending on where the TB bacteria grow.
Tuberculosis can spread when a person with the illness coughs, sneezes or sings. This can put tiny droplets with the germs into the air. Another person can then breathe in the droplets, and the germs enter the lungs.
Tuberculosis spreads easily where people gather in crowds or where people live in crowded conditions. People with HIV/AIDS and other people with weakened immune systems have a higher risk of catching tuberculosis than people with typical immune systems.
Antibiotics can treat tuberculosis. But some forms of the bacteria no longer respond well to treatments.
Table of Contents
Stages and Symptoms of tuberculosis
When tuberculosis (TB) germs survive and multiply in the lungs, it is called a TB infection. A TB infection may be in one of three stages. Symptoms are different in each stage.
Primary TB infection
The first stage is called the primary infection. Immune system cells find and capture the germs. The immune system may completely destroy the germs. But some captured germs may still survive and multiply.
Most people don’t have symptoms during a primary infection. Some people may get flu-like symptoms, such as:
- Cough.
- Tiredness.
- Low fever.
Latent TB infection
Primary infection is usually followed by the stage called latent TB infection. Immune system cells build a wall around lung tissue with TB germs. The germs can’t do any more harm if the immune system keeps them under control. But the germs survive. There are no symptoms during latent TB infection.
Active TB disease
Active TB disease happens when the immune system can’t control an infection. Germs cause disease throughout the lungs or other parts of the body. Active TB disease may happen right after primary infection. But it usually happens after months or years of latent TB infection.
Symptoms of active TB disease in the lungs usually begin gradually and worsen over a few weeks. They may include:
- Cough.
- Coughing up blood or mucus.
- Chest pain.
- Pain with breathing or coughing.
- Fever.
- Chills.
- Night sweats.
- Weight loss.
- Not wanting to eat.
- Tiredness.
- Not feeling well in general.
Active TB disease outside the lungs
TB infection can spread from the lungs to other parts of the body. This is called extrapulmonary tuberculosis. Symptoms vary depending on what part of the body is infected. Common symptoms may include:
- Fever.
- Chills.
- Night sweats.
- Weight loss.
- Not wanting to eat.
- Tiredness.
- Not feeling well in general.
- Pain near the site of infection.
Active TB disease in the voice box is outside the lungs, but it has symptoms more like disease in the lungs.
Common sites of active TB disease outside the lungs include:
- Kidneys.
- Liver.
- Fluid surrounding the brain and spinal cord.
- Heart muscles.
- Genitals.
- Lymph nodes.
- Bones and joints.
- Skin.
- Walls of blood vessels.
- Voice box, also called larynx.
Active TB disease in children
Symptoms of active TB disease in children vary. Typically, symptoms by age may include the following:
- Teenagers. Symptoms are similar to adult symptoms.
- 1- to 12-year-olds. Younger children may have a fever that won’t go away and weight loss.
- Infants.The baby doesn’t grow or gain weight as expected. Also, a baby may have symptoms from swelling in the fluid around the brain or spinal cord, including, Being sluggish or not active, Unusually fussy, Vomiting, Poor feeding, Bulging soft spot on the head, and poor reflexes.
Stages and symptoms of chronic obstructive pulmonary disease (COPD)
Causes of tuberculosis
A bacterium called Mycobacterium tuberculosis causes TB. A variety of TB strains exist, and some of these have become resistant to medication.
TB bacteria are transmitted through infected droplets in the air. Once these droplets enter the air, anyone nearby can inhale them. Someone with TB can transmit bacteria by:
- sneezing
- coughing
- speaking
- singing
People with well-functioning immune systems may not experience TB symptoms, even if they’ve contracted the bacteria. This is known as latent or inactive TB infection. Latent TB is not contagious, but it can become active disease over time. Active TB disease can make you sick, and you can also spread it to others.
A person with a latent TB infection cannot pass the disease to other people. A person taking drugs to treat active TB disease usually can’t pass the disease after 2 to 3 weeks of treatment.
In addition to active or inactive, you might hear about different kinds of TB, including the most common, pulmonary (lung) tuberculosis. But the bacterium can also affect other parts of your body besides the lungs, causing extrapulmonary tuberculosis (or TB outside of the lung). You might also hear about systemic miliary tuberculosis, which can spread throughout your body and cause:
- Meningitis, an inflammation of your brain.
- Sterile pyuria, or high levels of white blood cells in your urine.
- Pott’s disease, also called spinal tuberculosis or tuberculosis spondylitis.
- Addison’s disease, an adrenal gland condition.
- Hepatitis, a liver infection.
- Lymphadenitis in your neck, also called scrofula or TB lymphadenitis.
Causes and risk factors of asthma
Risk factors of tuberculosis
Anyone can get tuberculosis, but certain factors increase the risk of getting an infection. Risk factors that increase your chance of contracting the bacteria that causes TB disease include:
- having diabetes, end stage kidney disease, or certain cancers
- malnutrition
- using tobacco or alcohol for long periods of time
- a diagnosis of HIV or having another immune-system-compromising situation
Medications that suppress the immune system can also put people at risk of developing active TB disease. These include medications that help prevent organ transplant rejection.
Other medications that increase your risk of active TB include those taken to treat:
- cancer
- rheumatoid arthritis
- Crohn’s disease
- psoriasis
- lupus
Traveling to regions with high TB rates can also increase your risk of contracting the bacterial infection. These regions include:
- sub-Saharan Africa
- India
- Mexico and other Latin American countries
- China and many other Asian countries
- parts of Russia and other countries of the former Soviet Union
- islands of Southeast Asia
- Micronesia
Age and active TB disease
The risk of a TB infection becoming active TB disease changes with age.
- Under 5 years of age. Until children reach age 5, they have high risk of a TB infection becoming active TBdisease. The risk is greater for children under age 2. Tuberculosis in this age group often leads to serious disease in the fluid surrounding the brain and spinal column, called meningitis.
- Age 15 to 25. People in this age group have an increased risk of developing more-severe active TB disease in the lungs.
- Age 65 and older. The immune system weakens during older age. Older adults have a greater risk of active TB disease. Also, the disease may be more difficult to treat.
Complications of tuberculosis
If tuberculosis is left untreated, the complications may include:
- Coughing up blood in sputum
- Pleurisy – which causes pain during breathing
- Pleural effusion – accumulation of fluid in lungs
- Lung function damage
- Cardiac tamponade
- Laryngitis
Risk factors and complications of pneumonia
Prevention of tuberculosis
Even if the risk of TB is low where you live, it never hurts to be familiar with the things you can do to prevent contracting the TB bacteria or transferring the infection to others. A few important steps you can take include:
- connecting with a healthcare professional for testing if you believe you’ve been exposed to TB
- getting tested for TB if you have HIV or any condition that increases your risk for infection
- visiting a travel clinic or check with your doctor about testing before and after traveling to a country with a high TB rate
- asking about your workplace infection prevention and control program and follow the precautions provided if your job carries a risk of exposure to TB
- avoiding close or prolonged contact with someone who has active TB
Preventing the spread of tuberculosis
If you have active TB disease, you’ll need to take steps to prevent other people from getting an infection. You will take drugs for four, six or nine months. Take all of the drugs as directed during the entire time.
During the first 2 to 3 weeks, you will be able to pass TB bacteria to others. Protect others with these steps:
- Stay home. Don’t go to work or school.
- Isolate at home. Spend as little time as possible among members of your household. Sleep in a separate room.
- Ventilate the room. Tuberculosis germs spread more easily in small, closed spaces. If it’s not too cold outdoors, open the windows. Use a fan to blow air out. If you have more than one window, use one fan to blow air out and another to blow air in.
- Wear face masks. Wear a mask when you have to be around other people. Ask other members of the household to wear masks to protect themselves.
- Cover your mouth. Use a tissue to cover your mouth anytime you sneeze or cough. Put the dirty tissue in a bag, seal it and throw it away.
- Get vaccinated. In countries where tuberculosis is common, infants often are vaccinated with the bacille Calmette-Guerin (BCG) vaccine. This protects infants and toddlers who are more likely to have active TBdisease in the fluid surrounding the brain and spinal cord.
Diagnosis of tuberculosis
To diagnosis a tuberculosis (TB) infection, your health care provider will do an exam that includes:
- Listening to you breathe with a stethoscope.
- Checking for swollen lymph nodes.
- Asking you questions about your symptoms.
Your health care provider will order tests if:
- Tuberculosis is suspected.
- You were likely exposed to a person with active tuberculosis (TB) disease.
- You have health risks for active TB disease.
Tests to diagnose TB include a skin test, a blood test, or both. You may need both if:
- a skin test is positive
- there’s a chance you’ve received a false negative result from the skin test.
A false negative result can happen if your immune system isn’t working properly or if it’s been less than 8 weeks since exposure to TB.
Your provider will determine whether a skin test or blood test is the best option.
Skin test
Your doctor can use a purified protein derivative (PPD) skin test to determine if you’ve acquired TB bacteria.
For this test, your doctor will inject 0.1 milliliter (mL) of PPD (a small amount of protein) under the top layer of your skin. Between 2 and 3 days later, you’ll return to your doctor’s office to have the results read.
A welt on your skin over 5 millimeters (mm) in size where the PPD was injected may be considered a positive result. Reactions between 5 and 15 mm in size can be considered positive depending on risk factors, health, and medical history. All reactions over 15 mm are considered positive, regardless of risk factors.
The test is not perfect, though. It can only tell you whether you have a TB infection, not whether you have active TB disease. Plus, some people do not respond to the test even if they have TB. Others respond to the test and do not have TB. People who’ve recently received the TB vaccine may test positive but not have a TB infection.
Blood test
Your doctor can use a blood test to follow up on TB skin results. They may also recommend a blood test first, particularly if you have an existing health condition that may affect your response to the skin test.
Blood tests results can be positive, negative, or indeterminate. Like the skin test, the blood test can’t indicate whether or not you have active TB disease.
Chest X-ray
If you get a positive result from the skin or blood test, your doctor will likely order a chest X-ray to look for certain small spots in your lungs. These spots, a sign of a TB infection, indicate that your body is trying to isolate the TB bacteria.
A negative chest X-ray can suggest latent TB, but it’s also possible your test results were incorrect. Your doctor may recommend other testing.
If the test indicates you have active TB disease, you will begin treatment for active TB. Otherwise, your doctor may recommend getting treated for latent TB. This can prevent the bacteria from reactivating and making you sick in the future.
Sputum tests
Your health care provider may take a sample of the mucus that comes up when you cough, also called sputum. If you have active TB disease in your lungs or voice box, lab tests can detect the bacteria.
A relatively quick laboratory test can tell if the sputum likely has the TB bacteria. But it may be showing bacteria with similar features.
Another lab test can confirm the presence of TB bacteria. The results often take several weeks. A lab test also can tell if it’s a drug-resistant form of the bacteria. This information helps your health care provider choose the best treatment.
Other lab tests
Other lab tests that may be ordered include:
- Breath test.
- Procedure to remove sputum from your lungs with a special tube.
- Urine test.
- Test of the fluid around the spine and brain, called cerebrospinal fluid.
Prevention and diagnosis of chronic cough
Treatment of tuberculosis
If you have a latent TB infection, your health care provider may begin drug treatments. This is especially true for people with HIV/AIDS or other factors that increase the risk of active TB disease. Most latent TB infections are treated for three or four months.
Active TB disease may be treated for four, six or nine months. Specialists in TBtreatment will determine which drugs are best for you.
Most common TB drugs
If you have a latent TB infection, you might need to take only one or two types of drugs. Active TB disease requires taking several drugs. Common medications used to treat tuberculosis include:
- Isoniazid.
- Rifampin (Rimactane).
- Rifabutin (Mycobutin).
- Rifapentine (Priftin).
- Pyrazinamide.
- Ethambutol (Myambutol).
You may be prescribed other drugs if you have drug-resistant tuberculosis or other complications from your illness.
Side effects of medications
Most people can take TB drugs without serious side effects. If you have serious side effects, your care provider may ask you to stop taking a drug. You may have to change the dose of a drug.
Talk to your health care provider if you experience any of the following:
- Upset stomach.
- Vomiting.
- Loss of appetite.
- Severe diarrhea.
- Light-colored stool.
- Dark urine.
- Yellowish skin or eye color.
- Changes in vision.
- Dizziness or trouble with balance.
- Tingling in hands or feet.
- Easy bruising or bleeding.
- Unexplained weight loss.
- Unexplained tiredness.
- Sadness or depression.
- Rash.
- Joint pain.
It is important for you to list all drugs, dietary supplements or herbal remedies you take. You may need to stop taking some of these during your treatment.
Drug-resistant TB
Some forms of the TB bacteria have become drug resistant. This means that drugs that once cured the disease no longer work.
This happens, in part, because of naturally occurring genetic changes in bacteria. A random genetic change in a bacterium might give it some quality that makes it more likely to survive the attack of an antibiotic. If it does survive, then it can multiply.
When antibiotic drugs aren’t used correctly or drugs fail to kill all the bacteria for another reason the conditions are ideal for more-resistant versions of the bacteria to get established and multiply. If these bacteria are passed on to other people, a new drug-resistant strain can grow over time.
Problems that can lead to such drug-resistant strains of bacteria include the following:
- People didn’t follow directions for taking the drugs or stopped taking the drugs.
- They weren’t prescribed the right treatment plan.
- Drugs were not available.
- The drugs were of poor quality.
- The body didn’t absorb the drugs as expected.
Tuberculosis vaccination
A TB vaccine, called the bacillus Calmette-Guérin (BCG) vaccine, is mostly used in countries with a high prevalence of TB. This vaccine works better for children than for adults.
- List of Common Diseases & Medical Disorders
- Buy Complete Premium Anatomy Notes (PDFs)
- Medmichihealthcare New posts
- Read All causes of disease short notes
- Read All diagnosis of disease short notes
- Read All treatment of disease short notes
- Subscribe Medmichihealthcare YouTube channel
Discover more from Medmichihealthcare
Subscribe to get the latest posts sent to your email.