Syncope is a term used for fainting or passing out. It is a medical condition that happens when you have a sudden, temporary drop in the amount of blood that flows to your brain. Most of the time, a harmless, short-term cause makes you faint.
The following are some of the reasons you could experience fainting:
- Changes in the amount of blood in the areas of your body.
- A sudden drop in blood pressure.
- A drop in your heart rate.
When you experience a pass out, you’ll likely become conscious and alert after a few seconds or minutes. However, you may feel confused or tired for a bit. You can recover fully in minutes or hours.
Fainting can be the first and only warning sign prior to an episode of sudden cardiac death. It can also lead to serious injury. Talk to your physician if it happens more often.
Table of Contents
What is pre-syncope
Pre-syncope is the feeling that you are about to pass out. Someone with pre-syncope may be lightheaded (dizzy) or nauseated, have a visual “gray out” or trouble hearing, have palpitations, or feel weak or suddenly sweaty. When discussing your fainting with your doctor, you should note episodes of pre-syncope as well.
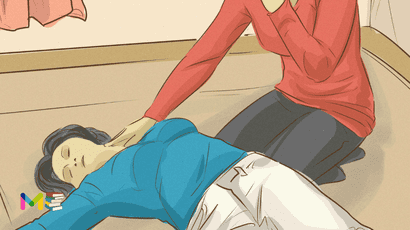
Somebody who faints should be moved and make sure they are lying down so blood could properly flow to their brain. If they do not regain consciousness promptly, start CPR.
Types of syncope
The following are the different types of fainting:
- Situational syncope happens only during certain situations that affect your nervous system and lead to fainting.
- Vasovagal syncope. happens when you have a sudden drop in blood pressure, which causes a drop in blood flow to your brain. It often occurs after standing for a while or under emotional distress.
- Postural syncope (also called postural hypotension or orthostatic hypotension) happens when your blood pressure drops suddenly due to a quick change in position, such as standing up after lying down.
- Cardiac syncope can occur if you have a heart or blood vessel condition that affects blood flow to your brain.
- Neurologic syncope can happen when you have a neurological condition such as a seizure, stroke or transient ischemic attack (TIA).
- Fainting caused by Postural orthostatic tachycardia syndrome (POTS).
- Unknown causes of fainting.
You can also read about signs and symptoms of asthma.
Symptoms of syncope
You may experience several symptoms shortly before you pass out. This symptoms can include:
- cold or clammy skin
- feeling dizzy or lightheaded
- feelings of weakness or unsteadiness
- headache
- nausea
- changes in vision, such as blurry vision, tunnel vision, or seeing spots
- ringing in the ears
- yawning or feeling tired
- blacking out
What to do during pre-syncope
- If you’re feeling dizzy and about to faint, lie down. Position yourself so your head is low and your legs are raised. This can help increase the blood flow to your brain. Lying down also lowers your risk of injury if you were to faint.
- If you are unable to lie down, sit down. Depending on the situation, you may not be able to lie down. In this case, sit down and put your head between your knees to increase the blood flow to your brain.
- Stay lying down or seated until the feelings of faintness has pass. Don’t get up too quickly, as this may make you feel faint again.
Not all cases of fainting are serious. However, it’s still a good idea to get medical attention when you experience one and also seek for help, like somebody who can drive you to the clinic.
Causes of syncope
Fainting or passing out, happens when you don’t have enough blood flowing to your brain. There are many causes for this, depending on the types. Many people have a medical condition they may or may not know about, that affects their nervous system or heart. You may also have a condition that affects blood flow through your body and causes your blood pressure to drop when you change positions (for example, going from lying down to standing).
The following are the causes of fainting accordingly:
Situational syncope
This happens only during certain situations that affect your nervous system and lead to passing out. Some of these situations are:
- Intense emotional stress.
- Dehydration.
- Anxiety.
- Fear.
- Pain.
- Hunger.
- Use of alcohol or drugs.
- Hyperventilation (breathing in too much oxygen and getting rid of too much carbon dioxide too quickly).
- Urinating (micturition syncope).
- Coughing forcefully, turning your neck or wearing a tight collar (carotid sinus hypersensitivity).
Vasovagal syncope
This happens when you have a sudden drop in blood pressure, which causes a drop in blood flow to your brain. It often occurs after standing for a while or under emotional distress. Normally, when you stand up, gravity makes blood settle in the lower part of your body, below your diaphragm. When that happens, your heart and autonomic nervous system work to keep your blood pressure stable.
In this type of fainting, your heart rate and blood pressure inappropriately decrease severely. This causes decreased blood flow to your brain and leads to passing out. Typically, this type of fainting is benign.
Postural syncope
This happens when your blood pressure drops suddenly due to a quick change in position, such as standing up after lying down. Certain medications and dehydration can lead to this condition. People with this type of syncope usually have changes in their blood pressure that cause it to drop by at least 20 millimeters of mercury (systolic/top number) and at least 10 millimeters of mercury (diastolic/bottom number) when they stand.
Cardiac syncope
This can occur if you have a heart or blood vessel condition that affects blood flow to your brain. These conditions can include:
- Abnormal heart rhythm (arrhythmia).
- Obstructed blood flow in your heart because of your heart’s structure (hypertrophic cardiomyopathy).
- Blockage in your heart’s blood vessels (myocardial ischemia).
- Valve disease.
- Aortic stenosis (narrowing).
- Blood clot.
- Heart failure.
If you experience this kind of fainting, it’s important to see a cardiologist for proper treatment.
Neurologic syncope
This can happen when you have a neurological condition such as a seizure, stroke or transient ischemic attack (TIA). Other less common conditions that lead to neurologic fainting include migraines and normal pressure hydrocephalus.
Postural orthostatic tachycardia syndrome
Postural orthostatic tachycardia syndrome (increased heart rate when standing), or POTS, is a rare clinical syndrome characterized by an increase in heart rate of at least 30 beats per minute on standing and orthostatic intolerance when standing brings on symptoms such as palpitations, lightheadedness and fatigue. POTS generally appears in young women. After excluding other causes, the diagnosis is made on physical examination, medical history and tilt-table test.
Treatment usually consists of increased salt and fluid intake, recumbent exercise (not standing upright) and education in avoiding triggers. POTS does not usually get worse with age.
Unknown causes of fainting
The cause of fainting is unknown in about 33% of people who have it. However, an increased risk of fainting is a side effect of some medications. Be sure to follow up with a provider if you don’t know what is causing you to pass out.
You can also read about causes and prevention of stroke.
Prevention of syncope
The following are the tips and remedies that can help you prevent passing out:
- Drink plenty of fluids. This may help prevent fainting due to dehydration.
- Don’t skip meals. You may want to eat smaller, more frequent meals throughout the day.
- Understand if there are external factors or triggers that may cause you to faint. This could include the sight of blood, getting an injection, or intense pain. If possible, try to avoid situations that may trigger a fainting episode.
- Avoid shirts with tight collars. This can help prevent carotid sinus syncope.
- Take your time when standing up. Standing up too quickly can cause a drop in blood pressure and prevent enough blood from flowing to your brain.
Diagnosis of syncope
It’s important to identify the cause of fainting, if possible, to rule out a dangerous heart condition. Depending on your symptoms and circumstances, the following tests may be used to find the cause:
- Exercise stress test: ECG recorded while strenuously exercising
- Electrocardiogram (ECG or EKG): wires taped to various parts of your body to create a graph of your heart’s electrical rhythm
- Echocardiogram or transesophageal echocardiogram: ultrasound of the heart
- Physical examination, including orthostatic vital signs and carotid sinus massage
- Tilt table test: measurement of heart rate and blood pressure in response to upright tilt, which simulates prolonged standing
- Electrophysiology study (EP): test that examines the heart’s electrical activity from the inside; used to diagnose many heart rhythm disorders
Self test monitors:
- Event monitor: a portable ECG you wear for one or two months, which records only when triggered by an abnormal heart rhythm or when you manually activate it
- Holter monitor: a portable ECG you wear continuously for one to seven days to record your heart rhythms over time
You can also read about diagnosis and treatment of high blood pressure.
Treatment of syncope
Treatment options will depend on what’s causing your fainting and the results of your evaluation and testing. The goal of treatment is to keep you from having episodes of fainting.
Fainting treatment options include:
- Making changes to your diet. Your provider may suggest that you eat small, frequent meals, eat more salt (sodium), drink more fluids, increase the amount of potassium in your diet and avoid caffeine and alcohol.
- Taking medications or making changes to medications you already take.
- Wearing support garments or compression stockings to improve blood circulation.
- Being extra cautious when you stand up.
- Elevating the head of your bed while you sleep. To do this, you can use extra pillows or place risers under the legs of the head of the bed.
- Avoiding or changing the situations or “triggers” that cause a syncope episode (avoiding standing for long periods of time, heat or emotional stressors).
- Biofeedback training to control a fast heartbeat.
- Getting treatment for structural heart disease.
- Getting a pacemaker to keep your heart rate regular (only for certain medical conditions).
- Getting an implantable cardioverter defibrillator (ICD). This device constantly monitors your heart rate and rhythm and corrects a fast, abnormal rhythm (only for certain medical conditions).
Medicines for fainting include:
- Fludrocortisone (Astonin or Florinef).
- Midodrine.
Side effects of the medication may include:
- Dizziness.
- Heartburn.
- Nausea.
- Urinary issues.
- Chills.
- Stomach issues.
If someone faints, follow these steps:
- Check to make sure they’re breathing.
- Make sure they lie down or sit with their head between their knees for at least 10 to 15 minutes.
- Offer the person cold water to drink.
Your doctor will develop a treatment plan that’s right for you and talk to you about your treatment options.
Depending on the cause of your painting, you should have a follow-up appointment with a provider for two to four weeks after you get hospital or outpatient treatment for it. If a provider discovers an issue with your heart’s structure or rhythm, you’ll need more follow-up appointments for that.
- List of Common Diseases & Medical Disorders
- Buy Complete Premium Anatomy Notes (PDFs)
- Medmichihealthcare New posts
- Read All causes of disease short notes
- Read All diagnosis of disease short notes
- Read All treatment of disease short notes
- Subscribe Medmichihealthcare YouTube channel
Discover more from Medmichihealthcare
Subscribe to get the latest posts sent to your email.