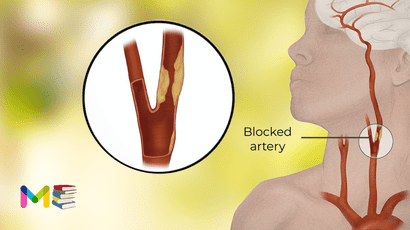
A stroke is a life-threatening condition that happens when part of your brain doesn’t have enough blood flow. This commonly happens because of a blocked artery or bleeding in your brain. Without a steady supply of blood, the brain cells in that area start to die from a lack of oxygen.
IMPORTANT: A stroke is a life-threatening emergency condition where every second counts. If you or someone with you has symptoms of a stroke, IMMEDIATELY call 911 (or your local emergency services number). The quicker stroke is treated, the more likely you’ll recover without disability.
To recognize the warning signs of a stroke, remember to think BE FAST:
- B. Be watchful for a sudden loss of balance.
- E. Look out for sudden loss of vision in one or both eyes. Are they experiencing double vision?
- F. Ask the person to smile. Look for a droop on one or both sides of their face, which is a sign of muscle weakness or paralysis.
- A. A person having a stroke often has muscle weakness on one side. Ask them to raise their arms. If they have one-sided weakness (and didn’t have it before), one arm will stay higher while the other will sag and drop downward.
- S. Strokes often cause a person to lose their ability to speak. They might slur their speech or have trouble choosing the right words.
- T. Time is critical, so don’t wait to get help! If possible, look at your watch or a clock and remember when symptoms start. Telling a healthcare provider when symptoms started can help the provider know what treatment options are best for you.
Table of Contents
What are the signs & symptoms of stroke
The loss of blood flow to the brain damages tissues within the brain. Symptoms of a stroke show up in the body parts controlled by the damaged areas of the brain.
The sooner a person having a stroke gets care, the better their outcome is likely to be. For this reason, it’s helpful to know the signs of stroke so you can act quickly. Stroke symptoms can include:
- Paralysis
- numbness or weakness in the arm, face, and leg, especially on one side of the body
- trouble speaking or understanding others
- slurred speech
- confusion, disorientation, or lack of responsiveness
- sudden behavioral changes, especially increased agitation
- vision problems, such as trouble seeing in one or both eyes with vision blackened or blurred, or double vision
- trouble walking
- loss of balance or coordination
- dizziness
- severe, sudden headache with an unknown
- cause
- seizures
- nausea or vomiting
A stroke requires immediate medical attention. If you think you or someone else is having a stroke, call 911 or local emergency services right away. Prompt treatment is key to preventing the following outcomes:
- brain damage
- long-term disability
- death
It’s better to be overly cautious when dealing with a stroke, so don’t be afraid to get emergency medical help if you think you recognize the signs of a stroke.
What are the types of stroke
There are two main causes of stroke: a blocked artery (ischemic stroke) or leaking or bursting of a blood vessel (hemorrhagic stroke). Some people may have only a temporary disruption of blood flow to the brain, known as a transient ischemic attack (TIA), that doesn’t cause lasting symptoms.
Ischemic stroke
Ischemia stroke is when cells don’t get enough blood flow to supply them with oxygen. This usually happens because something blocks blood vessels in your brain, cutting off blood flow. Ischemic strokes are the most common and account for about 80% of all strokes.
Ischemic strokes usually happen in one of the following ways:
- Formation of a clot in your brain (thrombosis.
- A fragment of a clot that formed elsewhere in your body that breaks free and travels through your blood vessels until it gets stuck in your brain (embolism).
- Small vessel blockage (lacunar stroke), which can happen when you have long-term, untreated high blood pressure (hypertension), high cholesterol (hyperlipidemia) or high blood sugar (Type 2 diabetes).
- Unknown reasons (these are cryptogenic strokes; the word “cryptogenic” means “hidden origin”).
Hemorrhagic stroke
Hemorrhagic stroke cause bleeding in or around your brain. This happens in one of two ways:
- Bleeding inside of your brain (intracerebral). This happens when a blood vessel inside of your brain tears or breaks open, causing bleeding that puts pressure on the surrounding brain tissue.
- Bleeding into the subarachnoid space (the space between your brain and its outer covering). The arachnoid membrane, a thin layer of tissue with a spiderweb-like pattern on it, surrounds your brain. The space between it and your brain is the subarachnoid space (“sub” means “under”). Damage to blood vessels that pass through the arachnoid membrane can cause a subarachnoid hemorrhage which is bleeding into the subarachnoid space, putting pressure on the brain tissue underneath.
Transient ischemic attack (TIA)
A transient ischemic attack (TIA) – sometimes known as a ministroke – is a temporary period of symptoms similar to those in a stroke. A TIA doesn’t cause permanent damage. A TIA is caused by a temporary decrease in blood supply to part of the brain, which may last as little as five minutes.
Like an ischemic stroke, a TIA occurs when a clot or debris reduces or blocks blood flow to part of the nervous system.
Seek emergency care even if you think you’ve had a TIA because your symptoms got better. It’s not possible to tell if you’re having a stroke or TIA based only on the symptoms. If you’ve had a TIA, it means you may have a partially blocked or narrowed artery leading to the brain. Having a TIA increases your risk of having a full-blown stroke later.
You can also read about symptoms and types of heart failure
What causes stroke
Ischemic strokes and hemorrhagic strokes can happen for many reasons. Ischemic strokes usually happen because of blood clots. These can happen for various reasons, such as:
- Atherosclerosis.
- Clotting disorders.
- Atrial fibrillation (especially when it happens due to sleep apnea).
- Heart defects (atrial septal defect or ventricular septal defect).
- Microvascular ischemic disease (which can block smaller blood vessels in your brain).
Hemorrhagic strokes can happen for several reasons also, including:
- High blood pressure, especially when you have it for a long time, when it’s very high, or both.
- Brain aneurysms can sometimes lead to hemorrhagic strokes.
- Brain tumors (including cancer).
- Diseases that weaken or cause unusual changes in blood vessels in your brain, such as moyamoya disease.
Other related conditions
Several other conditions and factors can contribute to a person’s stroke risk. These include:
- Alcohol use disorder.
- High blood pressure (this can play a role in all types of strokes, not just hemorrhagic ones because it can contribute to blood vessel damage that makes a stroke more likely).
- High cholesterol (hyperlipidemia).
- Migraine headaches (they can have symptoms similar to a stroke, and people with migraines especially migraines with auras – also have a higher risk of stroke at some point in their life).
- Type 2 diabetes.
- Smoking and other forms of tobacco use (including vaping and smokeless tobacco).
- Drug misuse (including prescription and nonprescription drugs).
Risk factors of stroke
Certain risk factors make you more susceptible to stroke. According to the National Heart, Lung, and Blood Institute, risk factors for stroke include:
Diet
An unbalanced diets can increase the risk of stroke. This type of diet is high in:
- salt
- saturated fats
- trans fats
- cholesterol
Inactivity
Inactivity, or lack of exercise, can also raise the risk of stroke.
Regular exercise has a number of health benefits. The CDC recommends that adults get at least 2.5 hrs of aerobic exercise every week. This can mean simply a brisk walk a few times a week.
Heavy alcohol use
The risk of stroke also increases with heavy alcohol consumption.
If you drink, drink in moderation. This means no more than one drink a day for women, and no more than two drinks a day for men.
Heavy alcohol use can raise blood pressure levels. It can also raise triglycerides levels, which can cause atherosclerosis. This is plaque buildup in the arteries that narrows blood vessels.
Tobacco use
Using tobacco in any form also raises the risk of stroke, since it can damage the blood vessels and heart. Nicotine also raises blood pressure.
Personal background
There are some risk factors for stroke you can’t control, such as:
- Family history. Stroke risk is higher in some families because of genetic health factors, such as high blood pressure.
- Sex. According to the CDC, while both women and men can have strokes, they’re more common in women than in men in all age groups.
- Age. The older you are, the more likely you are to have a stroke.
- Race and ethnicity. African Americans, Alaska Natives, and American Indians are more likely to have a stroke than other racial groups.
Health history
Certain medical conditions are linked to stroke risk. These include:
- a previous stroke or TIA
- high blood pressure
- high cholesterol
- carrying too much excess weight
- heart disorders, such as coronary artery disease
- heart valve defects
- enlarged heart chambers and irregular heartbeats
- sickle cell disease
- Diabetes
- blood clotting disorder
- patent foramen ovale (PFO)
To find out about your specific risk factors for stroke, talk with your doctor.
You can also read about causes and risk factors of heart attack
Complication of stroke
A stroke can sometimes cause temporary or permanent disabilities, depending on how long the brain lacks blood flow and which part is affected. Complications may include:
- Paralysis or loss of muscle movement. You may become paralyzed on one side of the body, or lose control of certain muscles, such as those on one side of the face or one arm.
- Difficulty talking or swallowing. A stroke might affect control of the muscles in the mouth and throat, making it difficult for you to talk clearly, swallow or eat. You also may have difficulty with language, including speaking or understanding speech, reading, or writing.
- Memory loss or thinking difficulties.Many people who have had strokes experience some memory loss. Others may have difficulty thinking, reasoning, making judgments and understanding concepts.
- Emotional problems. People who have had strokes may have more difficulty controlling their emotions, or they may develop depression.
- Pain. Pain, numbness or other unusual sensations may occur in the parts of the body affected by stroke. For example, if a stroke causes you to lose feeling in the left arm, you may develop an uncomfortable tingling sensation in that arm.
- Changes in behavior and self-care ability.People who have had strokes may become more withdrawn. They may need help with grooming and daily chores.
Prevention of stroke
There are many things you can do to reduce your risk of having a stroke. While this doesn’t mean you can prevent a stroke, it can lower your risk. Actions you can take include:
- Improve your lifestyle. Eating a healthy diet and adding exercise to your daily routine can improve your health. You should also make sure to get enough sleep (the recommended amount is seven to eight hours).
- Avoid risky lifestyle choices or make changes to your behaviors. Smoking and tobacco use, including vaping, recreational drug use or prescription drug misuse, and alcohol misuse can all increase your risk of having a stroke. It’s important to stop these or never start them. If you struggle with any of these, talking to your healthcare provider is important. Your provider can offer you guidance and resources that can help you change your lifestyle to avoid these behaviors.
- Manage your health conditions and risk factors. There are several conditions, such as obesity, abnormal heart rhythms, sleep apnea, high blood pressure, Type 2 diabetes or high cholesterol, which can increase your risk of having an ischemic stroke. If you have one or more of these conditions, it’s very important that you do what you can to manage them, especially by taking medications – such as blood thinners – as prescribed by your provider. Doing that earlier in life can you avoid severe stroke-related problems later in life.
- See your primary care provider for a checkup or wellness visit annually. Yearly wellness visits can detect health problems especially ones that contribute to having a stroke – long before you feel any symptoms.
If you’re at risk for any kind of stroke, your healthcare provider may recommend changing your diet to avoid increases in blood pressure. Examples of these include:
- Beverages that contain caffeine, such as coffee, tea, soft drinks, etc.
- Foods that contain a lot of salt or sodium, which can increase blood pressure.
- Foods that are high in saturated fats, such as fried foods, etc.
- Alcohol or recreational stimulant drugs (cocaine, amphetamines/methamphetamine, etc.).
You can also read about diagnosis and prevention of heart murmurs
Diagnosis of stroke
Your doctor will ask you or a family member about your symptoms and what you were doing when they arose. They’ll take your medical history to find out your stroke risk factors. They’ll also:
- ask what medications you take
- check your blood pressure
- listen to your heart
You’ll also have a physical exam, during which your doctor will evaluate you for:
- balance
- coordination
- weakness
- numbness in your arms, face, or legs
- signs of confusion
- vision issues
Your doctor will then do certain tests to help confirm a stroke diagnosis. These tests can help them determine whether you had a stroke and, if So:
- what may have caused it
- what part of the brain is affected
- whether you have bleeding in the brain
What tests will be done to diagnose stroke
The most common tests that happen when a healthcare provider suspects a stroke include:
- Computerized tomography (CT) scan.
- Lab blood tests (looking for signs of infections or heart damage, checking clotting ability and blood sugar levels, testing how well kidneys and liver function, etc.).
- Electrocardiogram (abbreviated ECG or EKG)
- to make sure that a heart issue isn’t the source of the problem.
- Magnetic resonance imaging (MRI) scans
- Electroencephalogram (EEG), though less common, can rule out seizures or related problems.
Treatment of stroke
Emergency treatment for stroke depends on whether you’re having an ischemic stroke or a stroke that involves bleeding into the brain (hemorrhagic).
Ischemic stroke
To treat an ischemic stroke, doctors must quickly restore blood flow to the brain. This may be done with:
- Emergency IV medication. Therapy with drugs that can break up a clot has to be given within 4.5 hours from when symptoms first started if given intravenously. The sooner these drugs are given, the better. Quick treatment not only improves your chances of survival but also may reduce complications. An IV injection of recombinant tissue plasminogen activator (TPA) – also called alteplase (Activase) or tenecteplase (TNKase) is the gold standard treatment for ischemic stroke. An injection of TPA is usually given through a vein in the arm within the first three hours. Sometimes, TPA can be given up to 4.5 hours after stroke symptoms started. This drug restores blood flow by dissolving the blood clot causing the stroke. By quickly removing the cause of the stroke, it may help people recover more fully from a stroke. Your doctor will consider certain risks, such as potential bleeding in the brain, to determine whether TPA is appropriate for you.
- Emergency endovascular procedures. Doctors sometimes treat ischemic strokes directly inside the blocked blood vessel. Endovascular therapy has been shown to significantly improve outcomes and reduce long-term disability after ischemic stroke. These procedures must be performed as soon as possible:
- Medications delivered directly to the brain. Doctors insert a long, thin tube (catheter) through an artery in the groin and thread it to the brain to deliver TPA directly where the stroke is happening. The time window for this treatment is somewhat longer than for injected TPA but is still limited.
- Removing the clot with a stent retriever. Doctors can use a device attached to a catheter to directly remove the clot from the blocked blood vessel in the brain. This procedure is particularly beneficial for people with large clots that can’t be completely dissolved with TPA. This procedure is often performed in combination with injected TPA.
Other procedures
To decrease your risk of having another stroke or transient ischemic attack, your doctor may recommend a procedure to open up an artery that’s narrowed by plaque. Options vary depending on the situation, these can include:
- Carotid endarterectomy. Carotid arteries are the blood vessels that run along each side of the neck, supplying the brain (carotid arteries) with blood. This surgery removes the plaque blocking a carotid artery and may reduce the risk of ischemic stroke. A carotid endarterectomy also involves risks, especially for people with heart disease or other medical conditions.
- Angioplasty and stents. In an angioplasty, a surgeon threads a catheter to the carotid arteries through an artery in the groin. A balloon is then inflated to expand the narrowed artery. Then a stent can be inserted to support the opened artery.
Hemorrhagic stroke
Emergency treatment of hemorrhagic stroke focuses on controlling the bleeding and reducing pressure in the brain caused by the excess fluid. Treatment options include:
- Emergency measures. If you take blood-thinning medications to prevent blood clots, you may be given drugs or transfusions of blood products to counteract the blood thinners’ effects. You may also be given drugs to lower the pressure in the brain (intracranial pressure), lower blood pressure, prevent spasms of the blood vessels and prevent seizures.
- Surgery. If the area of bleeding is large, your doctor may perform surgery to remove the blood and relieve pressure on the brain. Surgery may also be used to repair blood vessel problems associated with hemorrhagic strokes. Your doctor may recommend one of these procedures after a stroke or if an aneurysm, arteriovenous malformation (AM) or other type of blood vessel problem caused the hemorrhagic stroke.
- Surgical clipping. A surgeon places a tiny clamp at the base of the aneurysm to stop blood flow to it. This clamp can keep the aneurysm from bursting, or it can keep an aneurysm that has recently hemorrhaged from bleeding again.
- Coiling (endovascular embolization). Using a catheter inserted into an artery in the groin and guided to the brain, the surgeon will place tiny detachable coils into the aneurysm to fill it. This blocks blood flow into the aneurysm and causes blood to clot.
- Surgical AVM removal. Surgeons may remove a smaller AM if it’s located in an accessible area of the brain. This eliminates the risk of rupture and lowers the risk of hemorrhagic stroke. However, it’s not always possible to remove an AVM if it’s located deep within the brain, it’s large, or its removal would cause too much of an impact on brain function.
- Stereotactic radiosurgery. Using multiple beams of highly focused radiation, stereotactic radiosurgery is an advanced minimally invasive treatment used to repair blood vessel malformations.
Subscribe YouTube Channel
- Subscribe Medmichihealthcare YouTube channel
- List of Common Diseases & Medical Disorders
- Buy Complete Premium Anatomy Notes (PDFs)
- Medmichihealthcare New posts
- Read All causes of disease short notes
- Read All diagnosis of disease short notes
- Read All treatment of disease short notes
Discover more from Medmichihealthcare
Subscribe to get the latest posts sent to your email.