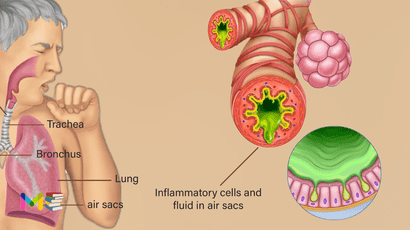
Pneumonia is an infection of the lungs, which is caused by bacteria, viruses or fungi. It causes the lung tissue to swell (inflammation) and can cause fluid or pus in the lungs. Bacterial pneumonia is usually more severe than viral one, which often resolves on its own.
This condition can range in seriousness from mild to life-threatening. It is most serious for infants and young children, people older than age 65, and people with health problems or weakened immune systems.
Study shows about millions of people is diagnosed with pneumonia each year in the United States. About 55,000 people die each year of it in the U.S. It’s the most common cause of death in developing countries.
Table of Contents
Symptoms of pneumonia
Symptoms can be mild to life threatening. They can include:
- fever
- coughing that may produce phlegm (mucus)
- sweating or chills
- shortness of breath that happens while doing normal activities, or even while resting
- chest pain that’s worse when you breathe or cough
- feelings of tiredness or fatigue
- loss of appetite
- headaches
- nausea or vomiting
Other symptoms can vary according to your age and general health:
- Older adults may have milder symptoms. They can also experience confusion or a lower-than-normal body temperature.
- Children under 5 years old may have fast breathing or wheezing.
- Infants may appear to have no symptoms, but sometimes they may vomit, lack energy, or have trouble drinking or eating.
When to see a healthcare provider:
See your doctor if you have difficulty breathing, chest pain, persistent fever of 102 F (39 C) or higher, or persistent cough, especially if you’re coughing up pus.
It’s especially important that people in these high-risk groups see a doctor:
- Adults older than age 65
- Children younger than age 2 with signs and symptoms
- People with an underlying health condition or weakened immune system
- People receiving chemotherapy or taking medication that suppresses the immune system
For some older adults and people with heart failure or chronic lung problems, it can quickly become a life-threatening condition.
You can also read about symptoms and causes of myocarditis (inflammation of the heart muscle).
Types of pneumonia
It is classified according to where and how it is acquired:
Community-acquired pneumonia
When you get pneumonia outside of a healthcare facility, it’s called community-acquired pneumonia. Causes include:
- Viruses: Viruses that cause the common cold, the flu (influenza), COVID-19 and respiratory syncytial virus (RSV) can sometimes lead to pneumonia.
- Bacteria: Infection with Streptococcus pneumoniae bacteria, also called pneumococcal disease, is the most common cause of CAP. Pneumococcal disease can also cause ear infections, sinus infections and meningitis. Mycoplasma pneumoniae bacteria causes atypical pneumonia, which usually has milder symptoms. Other bacteria that cause CAP include Haemophilus influenza, Chlamydia pneumoniae and Legionella (Legionnaires’ disease).
- Protozoa: Rarely, protozoa like Toxoplasma cause pneumonia.
- Fungi (molds): Fungi, like Cryptococcus, Pneumocystis jirovecii and Coccidioides, are uncommon causes of pneumonia. People with compromised immune systems are most at risk of getting pneumonia from a fungus.
Hospital-acquired pneumonia
You can get hospital-acquired pneumonia (HAP) while in a hospital or healthcare facility for another illness or procedure. HAP is usually more serious than community-acquired pneumonia because it’s often caused by antibiotic-resistant bacteria, like methicillin-resistant Staphylococcus aureus (MRSA). This means HAP can make you sicker and be harder to treat.
Healthcare-associated pneumonia
You can get healthcare-associated pneumonia while in a long-term care facility (such as a nursing home) or outpatient, extended-stay clinics. Like hospital-acquired pneumonia, it’s usually caused by antibiotic-resistant bacteria.
Ventilator-associated pneumonia
If you need to be on a respirator or breathing machine to help you breathe in the hospital (usually in the ICU), you’re at risk for ventilator-associated pneumonia (VAP). The same types of bacteria as community-acquired pneumonia, as well as the drug-resistant kinds that cause hospital-acquired pneumonia, cause VAP.
Aspiration pneumonia
Aspiration is when solid food, liquids, spit or vomit go down your trachea (windpipe) and into your lungs. If you can’t cough these up, your lungs can get infected.
Stages of pneumonia
It may be classified based off the area of the lungs it’s affecting:
- Bronchopneumonia: can affect areas throughout both of your lungs. It’s often localized close to or around your bronchi. These are the tubes that lead from your windpipe to your lungs.
- Lobar pneumonia: affects one or more lobes of your lungs. Each lung is made of lobes, which are defined sections of the lung.
Lobar pneumonia can be further divided into four stages based off how it’s progressed:
- Congestion. Lung tissue appears heavy and congested. Fluid filled with infectious organisms has accumulated in the air sacs.
- Red hepatization. Red bloods cells and immune cells have entered into the fluid. This makes the lungs appear red and solid in appearance.
- Gray hepatization. The red blood cells have begun to break down while immune cells remain. The breakdown of red blood cells causes a change in color, from red to gray.
- Resolution. Immune cells have begun to clear the infection. A productive cough helps eject remaining fluid from the lungs.
You can also read about types and classification of asthma.
Causes of pneumonia
Many germs can cause it. The most common are bacteria and viruses in the air we breathe. Your body usually prevents these germs from infecting your lungs. But sometimes these germs can overpower your immune system, even if your health is generally good.
It can develop when your immune system attacks an infection in the small sacs of your lung (alveoli). This causes your lungs to swell and leak fluids. Common illnesses that can lead to pneumonia include:
- Common cold (rhinovirus).
- The flu (influenza virus).
- Respiratory syncytial virus (RSV).
- COVID-19 (SARS-COV-2).
- Human metapneumovirus (HMPV).
- Human parainfluenza virus (HPIV).
- Legionnaires’ disease.
- Mycoplasma pneumonia bacteria.
- Pneumococcal disease.
- Pneumocystis pneumonia.
Pneumonia itself isn’t actually contagious, but the bacteria and viruses that cause it are. For instance, the flu is contagious and can lead to pneumonia, but most people who get the flu won’t get pneumonia.
The bacteria that most commonly causes pneumonia, Streptococcus pneumoniae, can be spread from person to person by touching infected surfaces or through coughing and sneezing.
Pneumonia caused by fungi isn’t contagious. Fungal infections aren’t spread from person to person like viruses and bacteria.
Risk factors of pneumonia
It can affect anyone. But the two age groups at highest risk are:
- People who are age 65 or older
- Children who are 2 years old or younger
Other risk factors include:
- Weakened or suppressed immune system. People who have HIV/AIDS, who’ve had an organ transplant, or who receive chemotherapy or long-term steroids are at risk.
- Chronic disease. You’re more likely to get pneumonia if you have asthma, chronic obstructive pulmonary disease (COPD) or heart disease.
- Smoking. Smoking damages your body’s natural defenses against the bacteria and viruses that cause pneumonia.
- Being hospitalized. You’re at greater risk of pneumonia if you’re in a hospital intensive care unit, especially if you’re on a machine that helps you breathe (a ventilator).
You can also read about causes and risk factors of heart failure.
Complications of pneumonia
It may cause complications, especially in people with weakened immune systems or chronic conditions, such as diabetes. Complications may include:
- Impaired breathing. You may have trouble getting enough oxygen when you breathe. You may need to use a ventilator.
- Worsened chronic conditions. If you have certain preexisting health conditions, pneumonia could make them worse. These conditions include congestive heart failure and emphysema. For certain people, pneumonia increases their risk of having a heart attack.
- Acute respiratory distress syndrome. This is a severe form of respiratory failure. It’s a medical emergency.
- Bacteremia. Bacteria from the pneumonia infection may spread to your bloodstream. This can lead to dangerously low blood pressure, septic shock, and, in some cases, organ failure.
- Pleural effusion. If your pneumonia isn’t treated, you may develop fluid around your lungs in your pleura, called pleural effusion. The pleura are thin membranes that line the outside of your lungs and the inside of your rib cage. The fluid may become infected and need to be drained.
- Lung abscesses. These are cavities in the lungs that contain pus. Antibiotics can treat them. Sometimes they may require drainage or surgery to remove the pus.
- Kidney, heart, and liver damage. These organs may be damaged if they don’t receive enough oxygen, or if there’s an overreaction of the immune system to the infection.
- Death. In some cases, pneumonia can be fatal. According to the CDC, nearly 44,000 people in the United States died from pneumonia in 2019.
Prevention of pneumonia
The best way to prevent it is to get vaccinated against bacteria and viruses that commonly cause it. There are also everyday precautions you can take to help reduce your risk.
There are two types of vaccines (shots) that prevent pneumonia caused by pneumococcal bacteria. Similar to a flu shot, these vaccines won’t protect against all types of pneumonia, but if you do get sick, it’s less likely to be severe.
- Childhood vaccinations: If you have children, ask their healthcare provider about other vaccines they should get. Several childhood vaccines help prevent infections caused by the bacteria and viruses that can lead to pneumonia.
- Vaccinations against viruses: As certain viruses can lead to pneumonia, getting vaccinated against COVID-19 and the flu can help reduce your risk of getting pneumonia.
- Pneumococcal vaccines: Pneumovax23® and Prevnar13® protect against pneumonia bacteria. They’re each recommended for certain age groups or those with increased risk for pneumonia. Ask your healthcare provider which vaccine would be appropriate for you or your loved ones.
In addition to getting vaccinated, you can reduce your risk of getting and spreading pneumonia with some healthy habits:
- Eat a healthy diet, exercise and get enough rest.
- Wash your hands with soap and water before eating, before handling food and after using the restroom. If soap isn’t available, use an alcohol-based hand sanitizer.
- Avoid close contact and sharing items with other people if either of you has an infectious disease such as the flu, a cold or COVID-19.
- If you have to stay in a hospital or other healthcare facility, don’t be afraid to ask your providers about how to reduce your risk of getting an infection during your stay.
- Get treated for any other infections or health conditions you may have. These conditions could weaken your immune system, which could increase your chance of pneumonia.
- Avoid excessive alcohol consumption.
- Quit smoking and avoid secondhand smoke. Smoking damages your lungs and makes you more likely to get an infection.
Diagnosis of pneumonia
Your provider may perform tests that look at your lungs for signs of infection, measure how well your lungs are working and examine blood or other body fluids to try to determine the cause of it. These include:
- Imaging: Your provider can use chest X-ray or CT scan to take pictures of your lungs to look for signs of infection.
- Blood tests: Your provider can use a blood test to help determine what kind of infection is causing your pneumonia.
- Sputum test: You’re asked to cough and then spit into a container to collect a sample for a lab to examine. The lab will look for signs of an infection and try to determine what’s causing it.
- Pulse oximetry: A sensor measures the amount of oxygen in your blood to give your provider an idea of how well your lungs are working.
- Pleural fluid culture: Your provider uses a thin needle to take a sample of fluid from around your lungs. The sample is sent to a lab to help determine what’s causing the infection.
- Arterial blood gas test: Your provider takes a blood sample from your wrist, arm or groin to measure oxygen levels in your blood to know how well your lungs are working.
- Bronchoscopy: In some cases, your provider may use a thin, lighted tube called a bronchoscope to look at the inside of your lungs. They may also take tissue or fluid samples to be tested in a lab.
You can also read about diagnosis and treatment of diabetes.
Treatment of pneumonia
Treatment depends on the cause, which can be bacterial, viral or fungal infection and how serious your case is. In many cases, the cause can’t be determined and treatment is focused on managing symptoms and making sure your condition doesn’t get worse. Treatment options include:
- Fever reducers/pain relievers. You may take these as needed for fever and discomfort. These include drugs such as aspirin, ibuprofen (Advil, Motrin IB, others) and acetaminophen (Tylenol, others).
- Cough medicine. This medicine may be used to calm your cough so that you can rest. Because coughing helps loosen and move fluid from your lungs, it’s a good idea not to eliminate your cough completely. In addition, you should know that very few studies have looked at whether over-the-counter cough medicines lessen coughing caused by pneumonia. If you want to try a cough suppressant, use the lowest dose that helps you rest.
- Antibiotics. These medicines are used to treat bacterial pneumonia. It may take time to identify the type of bacteria causing your pneumonia and to choose the best antibiotic to treat it. If your symptoms don’t improve, your doctor may recommend a different antibiotic.
- Antifungal medications: Antifungals can treat pneumonia caused by a fungal infection.
- Antiviral medications: Viral pneumonia usually isn’t treated with medication and can go away on its own. A provider may prescribe antivirals such as oseltamivir, zanamivir or peramivir to reduce how long you’re sick and how sick you get from a virus.
- Oxygen therapy: If you’re not getting enough oxygen, a provider may give you extra oxygen through a tube in your nose or a mask on your face.
- IV fluids: Fluids delivered directly to your vein (IV) treat or prevent dehydration.
- Draining of fluids: If you have a lot of fluid between your lungs and chest wall (pleural effusion), a provider may drain it. This is done with a catheter or surgery.
If you have a severe case or complications, you may need to stay in the hospital for treatment. You’re more likely to be hospitalized for treatment if you’re:
- Have a weakened immune system.
- Have health conditions that affect your heart and lungs
- Under age 2 or over age 65.
It may take six to eight weeks to feel back to normal if you’ve been hospitalized for treatment.
Viral pneumonia often goes away on its own, but you should always follow your healthcare provider’s recommendations to treat symptoms and reduce your risk of serious complications.
- List of Common Diseases & Medical Disorders
- Buy Complete Premium Anatomy Notes (PDFs)
- Medmichihealthcare New posts
- Read All causes of disease short notes
- Read All diagnosis of disease short notes
- Read All treatment of disease short notes
- Subscribe Medmichihealthcare YouTube channel
Discover more from Medmichihealthcare
Subscribe to get the latest posts sent to your email.