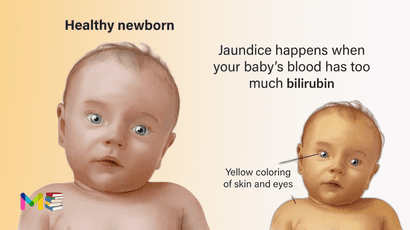
Newborn jaundice is the yellow discoloration of a newborn baby’s skin and eyes. It occurs because the baby’s blood contains an excess amount of bilirubin, a yellow pigment of red blood cells. Newborn jaundice is very common and usually goes away on its own. Sometimes babies need treatment with phototherapy.
Up to 60% of full-term babies develop jaundice during their first week of life. As many as 80% of premature babies develop jaundice during their first week of life.
Bilirubin is a yellow substance your body creates when red blood cells break down. While you’re pregnant, your liver removes bilirubin for your baby. But after birth, your baby’s liver must begin removing bilirubin. If your baby’s liver isn’t developed enough, it may not be able to get rid of bilirubin. When excess bilirubin builds up, your baby’s skin may appear yellow.
It’s important for your baby’s healthcare provider to check them for jaundice. Severe jaundice can lead to brain damage if it goes untreated.
Table of Contents
Types of newborn jaundice
There are a few different types of newborn jaundice. These include:
- Physiological jaundice. The most common type of newborn jaundice is physiological jaundice. This type of jaundice is normal. Physiological jaundice develops in most newborns by their second or third day of life. After your baby’s liver develops, it will start to get rid of excess bilirubin. Physiological jaundice usually isn’t serious and goes away on its own within two weeks.
- Breastfeeding jaundice. Jaundice is more common in breastfed babies than formula-fed babies. Breastfeeding jaundice frequently occurs during your baby’s first week of life. It happens when your baby doesn’t get enough breast milk. It can occur due to nursing difficulties or because your milk hasn’t come in yet. Breastfeeding jaundice may take longer to go away.
- Breast milk jaundice. Breast milk jaundice is different than breastfeeding jaundice. Substances in your breast milk can affect how your baby’s liver breaks down bilirubin. This can cause a bilirubin buildup. Breast milk jaundice may appear after your baby’s first week of life and may take a month or more to disappear.
- Other types of newborn jaundice can occur if your baby has an unrelated medication condition.
You can also read about types and symptoms of adults jaundice
Symptoms of newborn jaundice
The first sign of newborn jaundice is the yellowing of a baby’s skin and eyes, which may start in the face before spreading across the body. With physiological jaundice, the yellowing may begin and peak within 2 to 5 days after birth. With other causes, it may begin closer to birth.
However, this yellowing can be harder to see in darker skin tones. Another way to tell is by pressing your finger lightly on the baby’s skin. The spot should briefly appear paler. If it looks more yellow, it’s likely a sign of jaundice.
In many hospitals, birthing parents and newborns are discharge after 24-48 hours before jaundice may become very apparent. If the baby has not developed jaundice within 72 hours of delivery, they’re less likely to have the pathological form. But they can still develop the physiological form, leading to complications.
If you have concerns or are unsure, contact your baby’s doctor, particularly if the whites of your baby’s eyes look yellow, after you’re home.
The following signs or symptoms may indicate severe jaundice or complications from excess bilirubin. These include:
- Your baby’s skin becomes more yellow
- The skin on your baby’s the abdomen, arms or legs looks yellow
- The whites of your baby’s eyes look yellow
- Your baby seems listless or sick or is difficult to awaken
- Your baby isn’t gaining weight or is feeding poorly
- Your baby makes high-pitched cries
- Your baby develops any other signs or symptoms that concern you
Causes of newborn jaundice
Newborn jaundice happens when your baby’s blood has too much bilirubin. Bilirubin is a chemical your body makes when it breaks down old red blood cells. Your liver normally filters bilirubin from your blood. Your body gets rid of it when you poop.
If your baby’s liver hasn’t developed enough to get rid of bilirubin, it can start to build up. This buildup of bilirubin causes your baby’s skin to look yellow. Most babies develop jaundice in their first few days of life. This is because it takes a few days for your baby’s liver to develop and get better at removing bilirubin.
An underlying disorder may cause newborn jaundice. In these cases, jaundice often appears much earlier or much later than does the more common form of infant jaundice. Diseases or conditions that can cause jaundice include:
- Internal bleeding (hemorrhage)
- An infection in your baby’s blood (sepsis)
- Other viral or bacterial infections
- An incompatibility between the mother’s blood and the baby’s blood
- A liver malfunction
- Biliary atresia, a condition in which the baby’s bile ducts are blocked or scarred
- An enzyme deficiency
- An abnormality of your baby’s red blood cells that causes them to break down rapidly
- Bruising from a difficult birth
- A low oxygen level (hypoxia).
You can also read about symptoms and causes of liver cirrhosis
Risk factors of newborn jaundice
There are some things that can increase the chance of a newborn developing physiological jaundice. These include:
- premature birth
- history of newborn jaundice in siblings
- being male assigned at birth (MAAB)
- being of Asian descent
In addition, certain risk factors can increase your baby’s chance of developing severe jaundice, which may be physiological or pathological. These include:
- jaundice within 24 hours after birth
- birth before 40 weeks, with the chance increasing the earlier the baby is born
- treatment with phototherapy or a history of a sibling being treated with phototherapy for jaundice
- family history of inherited red blood cell disorders such as G6PD deficiency
- difficulty breastfeeding or chestfeeding
- bruising on the head or scalp from the birth
- having Down syndrome
- Being born bigger than average for gestational age (macrosomia)
Complications of newborn jaundice
High levels of bilirubin that cause severe jaundice can result in serious complications if not treated. These include:
Acute bilirubin encephalopathy. Bilirubin is toxic to cells of the brain. If a baby has severe jaundice, there’s a risk of bilirubin passing into the brain, a condition called acute bilirubin encephalopathy. Prompt treatment may prevent significant lasting damage.
Signs of acute bilirubin encephalopathy in a baby with jaundice include:
- Listlessness
- Difficulty waking
- High-pitched crying
- Poor sucking or feeding
- Backward arching of the neck and body
- Fever
Kernicterus. Kernicterus is the syndrome that occurs if acute bilirubin encephalopathy causes permanent damage to the brain. Kernicterus may result in:
- Involuntary and uncontrolled movements (athetoid cerebral palsy)
- Permanent upward gaze
- Hearing loss
- Improper development of tooth enamel
You can also read about risk factors and complications of eczema
Prevention of newborn jaundice
Newborn jaundice is normal and usually can’t be prevented. You can reduce the risk that your baby will develop severe jaundice by feeding them often. Frequent feedings stimulate regular bowel movements which will help your baby get rid of the bilirubin.
- Breastfed babies: You should breastfeed your baby eight to 12 times a day during their first week of life.
- Formula-fed babies: You should give your baby one to two ounces (30 to 60 milliliters) of formula every two to three hours during their first week of life. Ensure at least eight feeds in a 24-hour period.
Also, make sure your baby’s healthcare provider checks your baby’s bilirubin level before you leave the hospital. Schedule a follow-up visit during your baby’s first week of life to have the bilirubin level checked again.
Diagnosis of newborn jaundice
Your doctor will likely diagnose newborn jaundice on the basis of your baby’s appearance. However, it’s still necessary to measure the level of bilirubin in your baby’s blood. The level of bilirubin (severity of jaundice) will determine the course of treatment. Tests to detect jaundice and measure bilirubin include:
- A physical exam
- A laboratory test of a sample of your baby’s blood
- A skin test with a device called a transcutaneous bilirubinometer, which measures the reflection of a special light shone through the skin
- Coombs test. Additionally, this may be done to check for antibodies that show an elevated risk of increased red cell breakdown (hemolysis).
Your doctor may order other additional blood tests or urine tests if there’s evidence that your baby’s jaundice is caused by an underlying disorder.
You can also read about prevention and diagnosis of amniotic fluid deficiency
Treatment of newborn jaundice
Treatment for jaundice in newborns isn’t usually necessary. Mild levels of jaundice typically go away on their own as your baby’s liver continues to develop. This can take one to two weeks. Feeding your baby often (10 to 12 times a day) can encourage pooping (bowel movements). This helps your baby rid their body of the excess bilirubin.
If your baby’s bilirubin level is high or continues to rise, their healthcare provider may recommend the following treatment options. These include:
- Enhanced nutrition. To prevent weight loss, your doctor may recommend more-frequent feeding or supplementation to ensure that your baby receives adequate nutrition.
- Light therapy (phototherapy). Your baby may be placed under a special lamp that emits light in the blue-green spectrum. The light changes the shape and structure of bilirubin molecules in such a way that they can be excreted in both the urine and stool. During phototherapy treatment, your baby will wear only a diaper and protective eye patches. Light therapy may be supplemented with the use of a light-emitting pad or mattress.
- Intravenous immunoglobulin (IVIg). Jaundice may be related to blood type differences between mother and baby. This condition results in the baby carrying antibodies from the mother that contribute to the rapid breakdown of the baby’s red blood cells. Intravenous transfusion of an immunoglobulin, a blood protein that can reduce levels of antibodies, this may decrease jaundice and lessen the need for an exchange transfusion, although results are not conclusive.
- Exchange transfusion. Rarely, when severe jaundice doesn’t respond to other treatments, a baby may need an exchange transfusion of blood. This involves repeatedly withdrawing small amounts of blood and replacing it with donor blood, thereby diluting the bilirubin and maternal antibodies, a procedure that’s performed in a newborn intensive care unit.
When newborn jaundice isn’t severe, your doctor may recommend changes in feeding habits that can lower levels of bilirubin. Talk to your doctor if you have any questions or concerns about how much or how often your baby is feeding or if you’re having trouble breast-feeding.
- List of Common Diseases & Medical Disorders
- Buy Complete Premium Anatomy Notes (PDFs)
- Medmichihealthcare New posts
- Read All causes of disease short notes
- Read All diagnosis of disease short notes
- Read All treatment of disease short notes
- Subscribe Medmichihealthcare YouTube channel
Discover more from Medmichihealthcare
Subscribe to get the latest posts sent to your email.