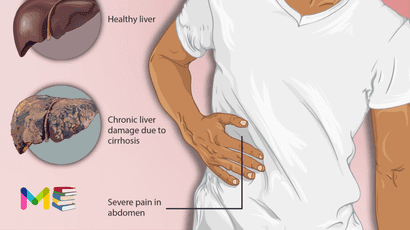
Liver cirrhosis is the late stage of liver disease, in which healthy liver tissue has been gradually replaced with scar tissue. This is a result of many forms of liver diseases and conditions, such as hepatitis or chronic alcoholism.
When inflammation is ongoing, your liver attempts to repair itself by scarring. But too much scar tissue prevents your liver from working properly. As cirrhosis gets worse, more and more scar tissue forms, making it difficult for the liver to do its job. The end stage is chronic liver failure.
The scarring that occurs with cirrhosis is usually irreversible, but treatment can help manage it.
Table of Contents
Symptoms of liver cirrhosis
Many times, there aren’t noticeable symptoms of cirrhosis until the condition has progressed.
Symptoms begin to occur because scarring on the liver has reached the point where the organ is limited in its ability to:
- break down toxins
- purify the blood
- help with the absorption of fats and fat-soluble vitamins
- produce clotting proteins
Some of the noticeable symptoms of liver cirrhosis include:
- fatigue
- decreased appetite
- unintentional weight loss
- mild pain on the upper right side of your abdomen
- nausea
- enlarged or swollen veins (varices or varicose veins)
- vomiting
More serious symptoms of liver cirrhosis include:
- yellow discoloration of your skin and eyes (jaundice)
- confusion and difficulty thinking clearly
- bruising or bleeding easily
- very itchy skin
- urine that looks darker than usual
- swelling of your legs (edema)
- abdominal swelling (ascites)
You can also read about 5 types of hepatitis.
Causes of liver cirrhosis
A wide range of diseases and conditions can cause damage to the liver and lead to cirrhosis. Some of the causes include:
- Ongoing viral hepatitis (hepatitis B, C and D).
- Long-term alcohol abuse.
- Nonalcoholic fatty liver disease, a condition in which fat accumulates in the liver.
- Hemochromatosis, a condition that causes iron buildup in the body.
- Autoimmune hepatitis, which is a liver disease caused by the body’s immune system.
- Destruction of the bile ducts caused by primary biliary cholangitis.
- Hardening and scarring of the bile ducts caused by primary sclerosing cholangitis.
- Wilson’s disease, a condition in which copper accumulates in the liver.
- Cystic fibrosis.
- Alpha-1 antitrypsin deficiency.
- Poorly formed bile ducts, a condition known as biliary atresia.
- Inherited disorders of sugar metabolism, such as galactosemia or glycogen storage disease.
- Medications, including methotrexate or isoniazid.
- Infection, such as syphilis or brucellosis.
- Alagille syndrome, a genetic digestive disorder.
Risk factors of liver cirrhosis
The following can increase your risk of developing cirrhosis of the liver:
- Have a history of heavy alcohol use.
- Are older than 50.
- Have a chronic viral hepatitis infection.
- Being overweight. Being obese increases your risk of conditions that may lead to cirrhosis, such as nonalcoholic fatty liver disease and nonalcoholic steatohepatitis.
- Have metabolic syndrome.
You can also read about causes and risk factors of appendicitis.
Stages of liver cirrhosis
The symptoms of cirrhosis fall into two technical stages:
- compensated cirrhosis
- decompensated cirrhosis.
If liver cirrhosis is diagnosed early enough and treated, it’s possible to reverse from the decompensated to compensated stage.
The difference between the two stages include:
- Compensated cirrhosis. This is the asymptomatic (showing no symptoms) stage. There may still be scarring on the liver, but it has not progressed enough to cause many, or any, symptoms.
- Decompensated cirrhosis. This is the stage where most of the symptoms like jaundice or ascites occur. This is a very serious stage. In some situations, if you’re able to manage the reason cirrhosis started in the first place (e.g., heavy drinking), you may be able to reverse your diagnosis back to compensated.
Complications of liver cirrhosis
Several complications of cirrhosis can include:
- Infections. If you have cirrhosis, your body may have a hard time fighting infections. Ascites can lead to bacterial peritonitis, a serious infection.
- High blood pressure in the veins that supply the liver. This condition is known as portal hypertension. Cirrhosis slows the regular flow of blood through the liver. This increases pressure in the vein that brings blood to the liver.
- Swelling in the legs and abdomen. The increased pressure in the portal vein can cause fluid to accumulate in the legs, called edema, and in the abdomen, called ascites. Edema and ascites also may happen if the liver can’t make enough of certain blood proteins, such as albumin.
- Enlargement of the spleen. Portal hypertension can cause the spleen to trap white blood cells and platelets. This makes the spleen swell, a condition known as splenomegaly. Fewer white blood cells and platelets in your blood can be the first sign of cirrhosis.
- Bleeding. Portal hypertension can cause blood to be redirected to smaller veins. Strained by the extra pressure, these smaller veins can burst, causing serious bleeding. Portal hypertension also may cause enlarged veins, called varices (VAIR-uh-seez), in the esophagus or the stomach. These varices also may lead to life-threatening bleeding. If the liver can’t make enough clotting factors, this also can contribute to continued bleeding.
- Malnutrition. Cirrhosis may make it more difficult for your body to process nutrients, leading to weakness and weight loss.
- Buildup of toxins in the brain. A liver damaged by cirrhosis can’t clear toxins from the blood as well as a healthy liver can. These toxins can then build up in the brain and cause mental confusion and difficulty concentrating. This is known as hepatic encephalopathy. With time, hepatic encephalopathy can progress to unresponsiveness or coma.
- Jaundice. Jaundice occurs when the diseased liver doesn’t remove enough bilirubin, a blood waste product, from your blood. Jaundice causes yellowing of the skin and whites of the eyes and darkening of urine.
- Bone disease. Some people with cirrhosis lose bone strength and are at greater risk of fractures.
- Acute-on-chronic cirrhosis. Some people end up experiencing multiorgan failure. Researchers now believe this is a complication in some people who have cirrhosis. However, they don’t fully understand what causes it.
- Increased risk of liver cancer. A large proportion of people who develop liver cancer have pre-existing cirrhosis.
You can also read about complications and prevention of lung cancer.
Prevention of liver cirrhosis
You might be able to prevent liver disease from progressing to cirrhosis by intervening earlier in the process. This depends on whether you’re aware of it and whether there are steps you can take to prevent it.
Many people don’t have symptoms in the early stages, but a routine health checkup could help bring it to light. This could give you the chance to make important changes or begin treatment.
Once you have cirrhosis, your liver won’t get better. But it won’t necessarily get worse. If you still have compensated cirrhosis with little to no symptoms or side effects, you may continue that way for some time.
If you can stop or minimize the inflammation causing cirrhosis, it may not progress to the decompensated stage. But you’ll have to continue to protect your liver for the rest of your life.
Diagnosis of liver cirrhosis
A healthcare provider will begin by physically examining you for signs and symptoms of cirrhosis of the liver. They’ll ask you about when your symptoms began and whether they’ve changed over time.
They’ll also ask questions about your medical history, what medications, herbs or supplements you take, and your diet and lifestyle. They’ll look for clues that might suggest a history of liver disease or liver damage.
The physical exam will look for signs such as:
- reddened palms
- skin or eyes that appear more yellowed in color
- hand tremors
- decreased alertness
- an enlarged liver or spleen
Tests can reveal how damaged the liver cirrhosis has become. Some of the tests used for evaluation of cirrhosis are:
- coagulation blood tests to see how quickly blood clots
- a complete blood count to look for anemia
- albumin tests to check for a protein produced in the liver
- alpha fetoprotein, a liver cancer screening
- liver function tests
Additional tests that can evaluate the liver include:
- an ultrasound scan of the liver
- an upper endoscopy to see if esophageal varices are present
- an MRI of the abdomen
- a liver biopsy, which is the most conclusive test for cirrhosis
- a CT scan of the abdomen
You can also read about diagnosis and treatment of high blood pressure.
Treatment of liver cirrhosis
The objectives of treating cirrhosis of the liver include:
- General diet and lifestyle measures to reduce stress on your liver.
- Managing the cause, if possible, to slow or reduce the damage.
- Managing or screening for complications of cirrhosis.
- As a last resort, liver transplantation.
In early cirrhosis, it may be possible to minimize damage to the liver by treating the underlying cause. The options include:
- Medicines to control hepatitis. Medicines may limit further damage to liver cells caused by hepatitis B or C through specific treatment of these viruses.
- Treatment for alcohol dependency.People with cirrhosis caused by excessive alcohol use should try to stop drinking. If stopping alcohol use is difficult, your health care provider may recommend a treatment program for alcohol addiction. If you have cirrhosis, it is very important to stop drinking since any amount of alcohol is toxic to the liver.
- Medicines to control other causes and symptoms of cirrhosis. Medicines may slow the progression of certain types of liver cirrhosis. For example, for people with primary biliary cholangitis that is diagnosed early, medicine may significantly delay progression to cirrhosis.
- Weight loss. People with cirrhosis caused by nonalcoholic fatty liver disease may become healthier if they lose weight and control their blood sugar levels.
- Other medicines. can relieve certain symptoms, such as itching, fatigue and pain. Nutritional supplements may be prescribed to counter malnutrition associated with cirrhosis. Supplements also can help prevent weak bones, known as osteoporosis.
Your health care provider will work with you to treat any complications of cirrhosis.
Medical procedure
In advanced cases of liver cirrhosis, when the liver stops working properly, a liver transplant may be the only treatment option. A liver transplant is a procedure to replace your liver with a healthy liver from a deceased donor or with part of a liver from a living donor. Cirrhosis is one of the most common reasons for a liver transplant. Candidates for liver transplant have extensive testing to determine whether they are healthy enough to have a good outcome following surgery.
Historically, those with alcoholic cirrhosis have not been liver transplant candidates because of the risk that they will return to harmful drinking after transplant. Recent studies, however, suggest that carefully selected people with severe alcoholic cirrhosis have post-transplant survival rates similar to those of liver transplant recipients with other types of liver disease.
For transplant to be an option if you have alcoholic cirrhosis, you would need to:
- Find a program that works with people who have alcoholic cirrhosis.
- Meet the requirements of the program. These would include lifelong commitment to alcohol abstinence as well as other requirements of the specific transplant center.
Scientists and healthcare professionals are working to expand current treatments for cirrhosis, but success has been limited. Because cirrhosis has a variety of causes and complications, there are many potential avenues of approach.
A combination of increased screening, lifestyle changes and new medicines may improve outcomes for people with liver problems or damage, if started early.
Subscribe YouTube Channel
- Subscribe Medmichihealthcare YouTube channel
- List of Common Diseases & Medical Disorders
- Buy Complete Premium Anatomy Notes (PDFs)
- Medmichihealthcare New posts
- Read All causes of disease short notes
- Read All diagnosis of disease short notes
- Read All treatment of disease short notes
Discover more from Medmichihealthcare
Subscribe to get the latest posts sent to your email.
Thanks dear.