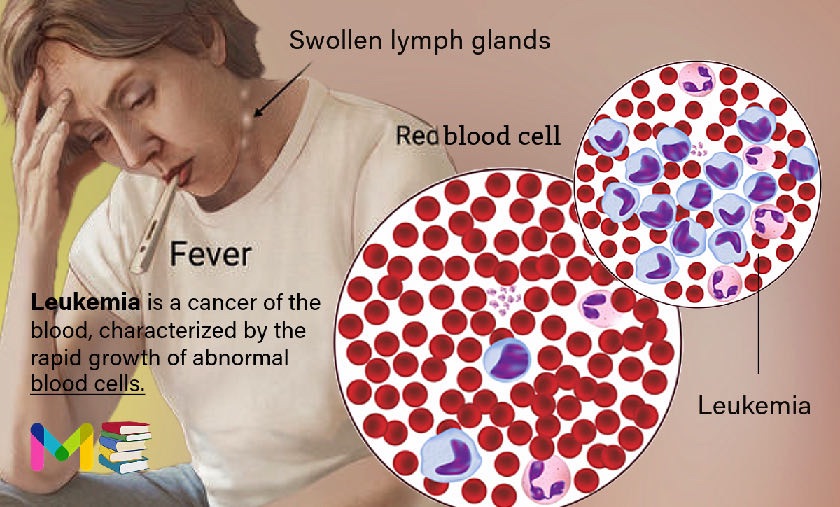
Leukemia is a cancer of the blood, characterized by the rapid growth of abnormal white blood cells. Leukemia starts when the DNA of a single cell in your bone marrow changes (mutates) and can’t develop and function normally. Leukemia also affects the lymphatic system.
White blood cells are potent infection fighters, they normally grow and divide in an orderly way, as your body needs them. But in people with leukemia, the bone marrow produces an excessive amount of abnormal white blood cells, which don’t function properly.
WBCs are a vital part of your immune system. They protect your body from invasion by:
- bacteria
- viruses
- fungi
- abnormal cells
- foreign substances
WBCs are mostly produced in the bone marrow, but certain types of WBCs are also made in the:
- lymph nodes
- spleen
- thymus gland
Once formed, WBCs travel through your bloodstream and lymphatic vessels to fight infection in the body’s tissues.
Unlike other cancers, leukemia doesn’t generally form a mass (tumor) that shows up in imaging tests, such as X-rays or CT scans.
Leukemia is the 10th most common cancer in the U.S., accounting for 3.2% of all new cancer cases. Leukemia can affect anyone, but it’s more common among people who are, ages 65 to 74, male, and caucasian/white.
Many types of leukemia exist. Some forms of leukemia are more common in children. Other forms of leukemia occur mostly in adults. Treatment depends on the type of leukemia and other factors.
Table of Contents
Key points about Leukemia
- Leukemia is cancer characterized by the rapid growth of abnormal white blood cells (WBC).
- There are four main types of leukemia. These include Acute lymphocytic leukemia (ALL), Acute myelogenous leukemia (AML), Chronic lymphocytic leukemia (CLL), and Chronic myelogenous leukemia (CML).
- Leukemia begins in bone marrow, the soft spongy tissue in the inner cavity of your bones, where your body’s blood cells are made.
- Leukemia can cause symptoms such as frequent infections, painless and swollen lymph nodes, bone pain and tenderness, fatigue and weakness, and more.
- Risk factors of leukemia may include blood disorders, exposure to certain chemicals, smoking, family history, and more.
- Treatments for leukemia depend on the type of leukemia you have, your age and overall health, and if the leukemia has spread to other organs or tissues. Treatments may include chemotherapy, immunotherapy, radiation therapy, and more.
Key points about lung cancer
Classifications of leukemia
Leukemia is classified based on how fast the disease worsens and whether leukemia cells arise from myeloid cells or lymphoid cells.
Leukemia by speed of disease progression
- Acute leukemia. The leukemia cells divide rapidly and the disease progresses quickly. If you have acute leukemia, you’ll feel sick within weeks of the leukemia cells forming. Acute leukemia is life-threatening and requires immediate initiation of therapy. Acute leukemia is the most common cancer in children.
- Chronic leukemia. Often, these leukemia cells behave as both immature and mature blood cells. Some cells develop to the point where they function as the cells they were meant to become, but not to the extent their normal counterparts do. The disease typically worsens slowly compared to acute leukemia. If you have chronic leukemia, you may not have noticeable symptoms for years. Chronic leukemia is more common in adults than in children.
Leukemia by cell type
- Myelogenous (mai-uh-lOW-juh-nuhs) or myeloid leukemia. This develops from myeloid cells. Normal myeloid cells develop into red blood cells, white blood cells and platelets.
- Lymphocytic leukemia. This develops from lymphoid cells. Normal lymphoid cells develop into white blood cells that are an important part of your body’s immuneI system.
Types of leukemia
There are four main types of leukemia:
- Acute lymphocytic leukemia (ALL). This is the most common type of leukemia in children, teens and young adults up to age 39. ALL can affect adults of any age.
- Acute myelogenous leukemia (AML). This is the most common type of acute leukemia in adults. It’s more common in older adults (those over 65). AML also occurs in children.
- Chronic lymphocytic leukemia (CLL). This is the most common chronic leukemia in adults (most common in people over 65). Symptoms may not appear for several years with CLL.
- Chronic myelogenous leukemia (CML). This is more common in older adults (most common in people over 65) but can affect adults of any age. It rarely occurs in children. Symptoms may not appear for several years with CML.
Read: Classification and types of hemophilia
Development of leukemia
Leukemia begins in bone marrow, the soft spongy tissue in the inner cavity of your bones, where your body’s blood cells are made. Blood cells go through multiple stages before reaching their fully mature forms. Mature, normal blood cells include:
- Red blood cells: Cells that carry oxygen and other vital materials to all tissues and organs in your body.
- White blood cells: Cells that fight infection.
- Platelets: Cells that help your blood clot.
These blood cells start as hematopoietic (hemo = blood, poiesis = make) stem cells. The stem cells develop into either myeloid (MAI-uh-loyd) cells or lymphoid (LIM-foyd) cells. If blood cells were to continue to develop normally, the mature forms of these cells are as follows:
- Myeloid cells develop into red blood cells, platelets and certain types of white blood cells (basophils, eosinophils and neutrophils).
- Lymphoid cells develop into certain white blood cells (lymphocytes and natural killer cells).
However, if you have leukemia, one of the developing blood cells begins to multiply out of control. These abnormal cells, called leukemia cells, begin to take over the space inside of your bone marrow. They crowd out the cells trying to develop into healthy red blood cells, white blood cells and platelets.
Symptoms of leukemia
The symptoms of leukemia may include:
- excessive sweating, especially at night (called “night sweats”)
- fatigue and weakness that do not go away with rest
- unintentional weight loss
- bone pain and tenderness
- painless, swollen lymph nodes (especially in the neck and armpits)
- enlarged liver or spleen
- red spots on the skin, called petechiae
- bleeding easily and bruising easily
- fever or chills
- frequent infections
Leukemia can also cause symptoms in organs that have been infiltrated or affected by the cancer cells. For example, if the cancer spreads to the central nervous system, it can cause:
- headaches
- nausea and vomiting
- confusion
- loss of muscle control
- seizures
How the cancer spreads depends on the type of leukemia and how aggressive it is.
Leukemia can also spread to other parts of your body, including the:
- lungs
- gastrointestinal tract
- heart
- kidneys
- testicles
Causes of leukemia
Leukemia starts when the DNA of a single cell in your bone marrow changes (mutates). DNA is the “instruction code” that tells a cell when to grow, how to develop and when to die. Because of the mutation, or coding error, leukemia cells keep multiplying. All cells arising from the original mutated cell also have the mutated DNA.
Scientists don’t know what causes these developing cells to mutate yet. They’ve been able to identify some common mutations that people diagnosed with different types of leukemia share.
Read: Symptoms and Causes of Arthritis
Risk factors of leukemia
Factors that may increase your risk of developing some types of leukemia include:
- Previous cancer treatment. People who’ve had certain types of chemotherapy and radiation therapy for other cancers have an increased risk of developing certain types of leukemia.
- Genetic disorders. Genetic abnormalities seem to play a role in the development of leukemia. Certain genetic disorders, such as Down syndrome, neurofibromatosis, Klinefelter syndrome, and Schwachman-Diamond syndrome are associated with an increased risk of leukemia.
- Blood disorders. Such as myelodysplastic syndrome, which is sometimes called “preleukemia”
- Exposure to certain chemicals. Exposure to certain chemicals, such as benzene. which is found in gasoline and is used by the chemical industry, is linked to an increased risk of some kinds of leukemia.
- Exposure to high levels of radiation
- Smoking. Smoking cigarettes increases the risk of acute myelogenous leukemia.
- Family history of leukemia. If members of your family have been diagnosed with leukemia, your risk of the disease may be increased.
However, most people with known risk factors don’t get leukemia. And many people with leukemia have none of these risk factors.
Diagnosis of leukemia
Leukemia may be suspected if you have concerning symptoms or certain risk factors. A doctor will begin by looking at your complete history and performing a physical examination.
Diagnostic exams and tests may include:
- Physical exam: Your healthcare provider will ask about your symptoms and feel for swollen lymph nodes and an enlarged spleen or liver. They may also inspect your gums for bleeding and swelling. They may look for a skin rash associated with leukemia that may appear red, purple or brown.
- Complete blood count (CBC): This blood test lets your healthcare provider know if you have abnormal levels of red blood cells, white blood cells and platelets. If you have leukemia, you’ll likely have higher than normal counts of white blood cells.
- Blood cell examination: Your healthcare provider may take additional blood samples to check for markers that indicate the presence of leukemia cells or a specific type of leukemia. Flow cytometry and peripheral blood smear are additional tests your healthcare provider may order.
- Bone marrow biopsy (bone marrow aspiration): Your healthcare provider may perform a biopsy if you have an abnormal white blood cell count. A long needle inserted into your bone marrow (usually in your pelvic bone) draws out fluid during the procedure. The fluid sample gets tested in a lab for leukemia cells. A bone marrow biopsy helps determine the percentage of abnormal cells in your bone marrow, confirming a leukemia diagnosis.
- Imaging and other tests: Your doctor may order a chest X-ray, CT scan, or magnetic resonance imaging (MRI) scan if symptoms indicate leukemia has affected your bones, organs or tissue. The leukemia cells don’t show up on imaging.
- Lumbar puncture (spinal tap): Your healthcare provider may test a sample of spinal fluid to see if leukemia has spread to the spinal fluid surrounding your brain and spinal cord.
Read: Risk Factors and Diagnosis of Dementia
Treatment of leukemia
Treatments for leukemia depend on the type of leukemia you have, your age and overall health, and if the leukemia has spread to other organs or tissues.
Leukemia is usually treated by a hematologist-oncologist. These are doctors who specialize in blood disorders and cancer.
Some forms of leukemia grow slowly and do not need immediate treatment. However, treatment for leukemia usually involves one or more of the following:
- Chemotherapy: Chemotherapy is the most common form of leukemia treatment. It involves using chemicals to kill leukemia cells or keep them from multiplying. During treatment, you may receive the chemicals (medication) as a pill, an injection into a vein or a shot under your skin. Usually, you’ll receive a combination of chemotherapy drugs.
- Immunotherapy (biologic therapy): This treatment uses certain drugs to boost your body’s defense system, your immune system, to fight leukemia. Immunotherapy helps your immune system identify cancer cells and produce more immune cells to fight them.
- Targeted therapy: This treatment uses drugs designed to attack specific parts of a leukemia cell (like a protein or gene) that are causing them to overtake normal blood cells. Targeted therapies may prevent leukemia cells from multiplying, cut off the cells’ blood supply or kill them directly. Targeted therapy is less likely to harm normal cells. Examples of targeted therapy drugs include monoclonal antibodies and tyrosine kinase inhibitors.
- Radiation therapy: This treatment uses strong energy beams or X-rays to kill leukemia cells or stop them from growing. During treatment, a machine directs radiation to the exact spots in your body where the cancer cells are or distributes radiation over your whole body. Distributing radiation throughout your body may happen before a hematopoietic cell transplant.
- Hematopoietic cell transplant (stem cell or bone marrow transplant): This treatment replaces the cancerous blood-forming cells killed by chemotherapy and/or radiation therapy with new, healthy hematopoietic cells. Your healthcare provider may remove these healthy cells from your blood or bone marrow before chemo and radiation, or they may come from a donor. The healthy new cells multiply, forming new bone marrow and blood cells that become the red blood cells, white blood cells and platelets your body needs.
- Chimeric antigen receptor (CAR) T-cell therapy: This is a novel type of therapy that takes your body’s infection-fighting T-cells (T-cell or T-lymphocyte is a type of immune cell), engineers them to fight leukemia cells and infuse them back into your body.
- Clinical trials. Clinical trials are experiments to test new cancer treatments and new ways of using existing treatments. While clinical trials give you or your child a chance to try the latest cancer treatment, treatment benefits and risks may be uncertain. Discuss the benefits and risks of clinical trials with your doctor.
Phases of leukemia treatment
Depending on your treatment plan, you may receive ongoing leukemia treatments long-term or treatment in phases. Generally, phased treatment involves three parts. Each phase has a specific goal.
- Induction therapy. The goal is to kill as many leukemia cells as possible in your blood and bone marrow to achieve remission. In remission, blood cell counts return to normal levels, no leukemia cells are found in your blood, and all signs and symptoms of the disease disappear. Induction therapy usually lasts four to six weeks.
- Consolidation (also called intensification). The goal is to kill any remaining undetected leukemia cells, so the cancer doesn’t return. You’ll usually receive consolidation therapy in cycles, over four to six months.
- Maintenance therapy. The goal is to kill any leukemia cells that may have survived the first two treatment phases and prevent the cancer from returning (relapse). Treatment lasts about two years.
Your healthcare provider may resume or change your treatment if the leukemia returns.
Read: Treatment of High Blood Pressure
The long-term outlook for people who have leukemia depends on the type of cancer they have and their stage at diagnosis. The sooner leukemia is diagnosed and the faster it’s treated, the better your chance of recovery is.
- List of Common Diseases & Medical Disorders
- Buy Complete Premium Anatomy Notes (PDFs)
- Medmichihealthcare New posts
- Read All causes of disease short notes
- Read All diagnosis of disease short notes
- Read All treatment of disease short notes
- Subscribe Medmichihealthcare YouTube channel
Discover more from Medmichihealthcare
Subscribe to get the latest posts sent to your email.