High blood pressure (also known as hypertension) occur when the force of blood pushing against your artery walls is consistently too high. This damages your arteries over time and can lead to serious complications like heart attack and stroke.
Blood pressure is measured in millimeters of mercury (mm Hg). In general, hypertension is a blood pressure reading of 130/80 millimeters of mercury (mm Hg) or higher.
- Normal blood pressure. Blood pressure is 120/80 mm Hg or lower.
- Elevated blood pressure. The top number ranges from 120 to 129 mm Hg and the bottom number is below, not above, 80 mm Hg.
- Stage 1 hypertension. The top number ranges from 130 to 139 mm Hg or the bottom number is between 80 and 89 mm Hg.
- Stage 2 hypertension. The top number is 140 mm Hg or higher or the bottom number is 90 mm Hg or higher.
Blood pressure higher than 180/120 mm Hg is considered a hypertensive emergency or crisis. Seek emergency medical help for anyone with these blood pressure numbers.
Untreated, high blood pressure increases the risk of heart attack, stroke and other serious health problems. It’s important to have your blood pressure checked at least every two years starting at age 18. Some people need more-frequent checks.
Healthy lifestyle habits —such as not smoking, exercising and eating well — can help prevent and treat high blood pressure. Some people need medicine to treat high blood pressure.
Table of Contents
Symptoms of high blood pressure
Hypertension is generally a silent condition. Many people won’t experience any symptoms. It may take years or even decades for the condition to reach levels severe enough that symptoms become obvious. Even then, these symptoms may be attributed to other issues.
Symptoms of severe hypertension can include:
- flushing
- blood spots in the eyes (subconjunctival hemorrhage)
- dizziness
The best way to know if you have hypertension is to get regular blood pressure readings. Most doctors’ offices take a blood pressure reading at every appointment.
If you only have a yearly physical, talk with your doctor about your risks for hypertension and other readings you may need to help you watch your blood pressure.
For example, if you have a family history of heart disease or have risk factors for developing the condition, your doctor may recommend that you have your blood pressure checked twice a year. This helps you and your doctor stay on top of any possible issues before they become problematic.
Types of high blood pressure
Your provider will diagnose you with one of two types of high blood pressure:
- Primary hypertension. Causes of this more common type of high blood pressure (about 90% of all adult cases in the U.S.) include aging and lifestyle factors like not getting enough exercise.
- Secondary hypertension. Causes of this type of high blood pressure include different medical conditions or a medication you’re taking.
Primary and secondary high blood pressure (hypertension) can co-exist. For example, a new secondary cause can make blood pressure that’s already high get even higher.
You might also hear about high blood pressure that comes or goes in certain situations. These hypertension types are:
- White coat hypertension: this is when your BP is normal at home but elevated in a healthcare setting.
- Masked hypertension: this is when your BP is normal in a healthcare setting but elevated at home.
- Sustained hypertension: this is when your BP is elevated in healthcare settings and at home.
- Nocturnal hypertension: this is when your BP goes up when you sleep.
You can also read about types and symptoms of stroke
Causes of high blood pressure
A combination of factors typically play a role in the development of primary hypertension:
- Genes: Some people are genetically predisposed to hypertension. This may be from gene mutations or genetic abnormalities inherited from your parents.
- Age: Individuals over 65 years old are more at risk for hypertension.
- Race: Black non-Hispanic individuals have a higher incidence of hypertension.
- Living with obesity: Living with obesity can lead to a few cardiac issues, including hypertension.
- High alcohol consumption: Women who habitually have more than one drink per day, and men who have more than two drinks per day, may be at an increased risk for hypertension.
- Living a very sedentary lifestlye: lowered levels of fitness have been connected to hypertension.
- Living with diabetes and/or metabolic syndrome: Individuals diagnosed with either diabetes or metabolic syndrome are at a higher risk of developing hypertension.
- High sodium intake: There’s a small association between daily high sodium intake (more than 1.5g a day) and hypertension.
Secondary hypertension often occurs quickly and can become more severe than primary hypertension. Several conditions that may cause secondary hypertension include:
- kidney disease
- obstructive sleep apnea
- congenital heart defects
- problems with your thyroid
- side effects of medications
- use of illegal drugs
- chronic consumption of alcohol
- adrenal gland problems
- certain endocrine tumors
You can also read about causes and symptoms of deep vein thrombosis
Risk factors of high blood pressure
Hypertension (high blood pressure) has many risk factors, including:
- Age. The risk of high blood pressure increases with age. Until about age 64, high blood pressure is more common in men. Women are more likely to develop high blood pressure after age 65.
- Race. High blood pressure is particularly common among Black people. It develops at an earlier age in Black people than it does in white people.
- Family history. You’re more likely to develop high blood pressure if you have a parent or sibling with the condition.
- Obesity or being overweight. Excess weight causes changes in the blood vessels, the kidneys and other parts of the body. These changes often increase blood pressure. Being overweight or having obesity also raises the risk of heart disease and its risk factors, such as high cholesterol.
- Lack of exercise. Not exercising can cause weight gain. Increased weight raises the risk of high blood pressure. People who are inactive also tend to have higher heart rates.
- Tobacco use or vaping. Smoking, chewing tobacco or vaping immediately raises blood pressure for a short while. Tobacco smoking injures blood vessel walls and speeds up the process of hardening of the arteries. If you smoke, ask your care provider for strategies to help you quit.
- Too much salt. A lot of salt — also called sodium — in the body can cause the body to retain fluid. This increases blood pressure.
- Low potassium levels. Potassium helps balance the amount of salt in the body’s cells. A proper balance of potassium is important for good heart health. Low potassium levels may be due to a lack of potassium in the diet or certain health conditions, including dehydration.
- Drinking too much alcohol. Alcohol use has been linked with increased blood pressure, particularly in men.
- Stress. High levels of stress can lead to a temporary increase in blood pressure. Stress-related habits such as eating more, using tobacco or drinking alcohol can lead to further increases in blood pressure.
- Certain chronic conditions. Kidney disease, diabetes and sleep apnea are some of the conditions that can lead to high blood pressure.
- Pregnancy. Sometimes pregnancy causes high blood pressure.
High blood pressure is most common in adults. But kids can have high blood pressure too. High blood pressure in children may be caused by problems with the kidneys or heart. But for a growing number of kids, high blood pressure is due to lifestyle habits such as an unhealthy diet and lack of exercise.
High blood pressure in pregnancy
When you have preeclampsia, your blood pressure is elevated (higher than 140/90 mmHg), and you may have high levels of protein in your urine. Preeclampsia puts stress on your heart and other organs and can cause serious complications. It can also affect the blood supply to your placenta, impair liver and kidney function or cause fluid to build up in your lungs. The protein in your urine is a sign of kidney dysfunction.
For people with risk factors, there are some steps that can be taken prior to and during pregnancy to lower the chance of developing preeclampsia. These steps can include:
- Losing weight if you have overweight/obesity (prior to pregnancy-related weight gain).
- Controlling your blood pressure and blood sugar (if you had high blood pressure or diabetes prior to pregnancy).
- Maintaining a regular exercise routine.
- Getting enough sleep.
- Eating healthy foods that are low in salt and avoiding caffeine.
If you have high blood pressure and are pregnant, discuss with your healthcare providers how to control blood pressure during your pregnancy.
Complications of high blood pressure
- Coronary artery disease (CAD).
- Stroke
- Heart attack.
- Peripheral artery disease.
- Kidney disease and kidney failure.
- Complications during pregnancy.
- Eye damage.
- Vascular dementia.
You can also read about risk factors and complications of heart attack
Diagnosis of high blood pressure
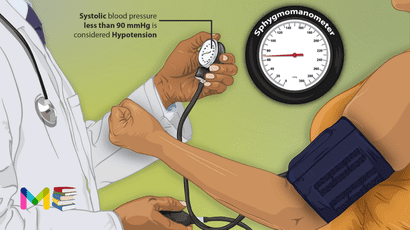
Diagnosing hypertension is as simple as taking a blood pressure reading. Most doctors’ offices check blood pressure as part of a routine visit. If you don’t receive a blood pressure reading at your next appointment, request one.
If your blood pressure is elevated, your doctor may request you have more readings over the course of a few days or weeks. A hypertension diagnosis is rarely given after just one reading.
Your doctor needs to see evidence of a sustained problem. That’s because your environment can contribute to increased blood pressure, like the stress you may feel by being at the doctor’s office. Also, blood pressure levels change throughout the day.
If your blood pressure remains high, your doctor will likely conduct more tests to rule out underlying conditions. These tests can include:
- cholesterol screening and other blood tests
- test of your heart’s electrical activity with an electrocardiogram (EKG, sometimes referred to as an ECG)
- ultrasound of your heart or kidneys
- home blood pressure monitor to monitor your blood pressure over a 24-hour period at home
These tests can help your doctor identify any secondary issues causing your elevated blood pressure. They can also look at the effects high blood pressure may have had on your organs.
During this time, your doctor may begin treating your hypertension. Early treatment may reduce your risk of lasting damage.
Prevention of high blood pressure
Fortunately, there are things you can do to reduce your risk of developing high blood pressure. These include:
- Cut down on sodium. To prevent hypertension, you should reduce the amount of sodium in your diet. Try to keep it below 1,500 milligrams a day.
- Follow a healthy eating plan. This is an important step in keeping your blood pressure normal. The DASH diet (Dietary Approaches to Stop Hypertension) emphasizes adding fruits, vegetables and whole grains to your diet.
- Keep a healthy weight. Going hand-in-hand with a proper diet is keeping a weight that’s healthy for you. Losing excess weight with diet and exercise will help lower your blood pressure to healthier levels.
- Drink alcohol in moderation. Having more than one drink a day (for women or people assigned female at birth) or more than two drinks a day (for men or people assigned male at birth) can raise blood pressure. One drink is defined as 1 ounce (oz) of alcohol, 5 ounces of wine or 12 ounces of beer.
- Keep active. Even simple physical activities, such as walking, can lower your blood pressure (and your weight).
Treatment for high blood pressure
Changing your lifestyle can help control and manage high blood pressure. Your health care provider may recommend that you make lifestyle changes including:
- Not smoking
- Limiting alcohol
- Eating a heart-healthy diet with less salt
- Maintaining a healthy weight or losing weight
- Getting 7 to 9 hours of sleep daily
- Getting regular physical activity
Sometimes lifestyle changes aren’t enough to treat high blood pressure. If they don’t help, your provider may recommend medicine to lower your blood pressure.
Medications for high blood pressure
The type of medicine used to treat hypertension depends on your overall health and how high your blood pressure is. Two or more blood pressure drugs often work better than one. It can take some time to find the medicine or combination of medicines that works best for you.
The ideal blood pressure goal can vary with age and health conditions, particularly if you’re older than age 65.
Medicines used to treat high blood pressure include:
- Water pills (diuretics). These drugs help remove sodium and water from the body. They are often the first medicines used to treat high blood pressure.There are different classes of diuretics, including thiazide, loop and potassium sparing. Which one your provider recommends depends on your blood pressure measurements and other health conditions, such as kidney disease or heart failure. Diuretics commonly used to treat blood pressure include chlorthalidone, hydrochlorothiazide (Microzide) and others.A common side effect of diuretics is increased urination. Urinating a lot can reduce potassium levels. A good balance of potassium is necessary to help the heart beat correctly. If you have low potassium (hypokalemia), your provider may recommend a potassium-sparing diuretic that contains triamterene.
- Angiotensin II receptor blockers (ARBs). These drugs also relax blood vessels. They block the action, not the formation, of a natural chemical that narrows blood vessels. angiotensin II receptor blockers (ARBs) include candesartan (Atacand), losartan (Cozaar) and others.
- Calcium channel blockers. These drugs help relax the muscles of the blood vessels. Some slow your heart rate. They include amlodipine (Norvasc), diltiazem (Cardizem, Tiazac, others) and others. Calcium channel blockers may work better for older people and Black people than do angiotensin-converting enzyme (ACE) inhibitors alone.Don’t eat or drink grapefruit products when taking calcium channel blockers. Grapefruit increases blood levels of certain calcium channel blockers, which can be dangerous. Talk to your provider or pharmacist if you’re concerned about interactions.
- Angiotensin-converting enzyme (ACE) inhibitors. These drugs help relax blood vessels. They block the formation of a natural chemical that narrows blood vessels. Examples include lisinopril (Prinivil, Zestril), benazepril (Lotensin), captopril and others.
Other medicines sometimes used to treat high blood pressure. If you’re having trouble reaching your blood pressure goal with combinations of the above medicines, your provider may prescribe:
- Alpha blockers. These medicines reduce nerve signals to blood vessels. They help lower the effects of natural chemicals that narrow blood vessels. Alpha blockers include doxazosin (Cardura), prazosin (Minipress) and others.
- Alpha-beta blockers. Alpha-beta blockers block nerve signals to blood vessels and slow the heartbeat. They reduce the amount of blood that must be pumped through the vessels. Alpha-beta blockers include carvedilol (Coreg) and labetalol (Trandate).
- Beta blockers. These medicines reduce the workload on the heart and widen the blood vessels. This helps the heart beat slower and with less force. Beta blockers include atenolol (Tenormin), metoprolol (Lopressor, Toprol-XL, Kapspargo sprinkle) and others.Beta blockers aren’t usually recommended as the only medicine prescribed. They may work best when combined with other blood pressure drugs.
- Aldosterone antagonists. These drugs may be used to treat resistant hypertension. They block the effect of a natural chemical that can lead to salt and fluid buildup in the body. Examples are spironolactone (Aldactone) and eplerenone (Inspra).
- Renin inhibitors. Aliskiren (Tekturna) slows the production of renin, an enzyme produced by the kidneys that starts a chain of chemical steps that increases blood pressure.Due to a risk of serious complications, including stroke, you shouldn’t take aliskiren with ACE inhibitors or ARBs.
- Vasodilators. These medicines stop the muscles in the artery walls from tightening. This prevents the arteries from narrowing. Examples include hydralazine and minoxidil.
- Central-acting agents. These medicines prevent the brain from telling the nervous system to increase the heart rate and narrow the blood vessels. Examples include clonidine (Catapres, Kapvay), guanfacine (Intuniv) and methyldopa.
Always take blood pressure medicines as prescribed. Never skip a dose or abruptly stop taking blood pressure medicines. Suddenly stopping certain ones, such as beta blockers, can cause a sharp increase in blood pressure called rebound hypertension.
If you skip doses because of cost, side effects or forgetfulness, talk to your care provider about solutions. Don’t change your treatment without your provider’s guidance.
Resistant hypertension
Resistant hypertension is a condition where your blood pressure remains high or unmanaged despite the medications you take to lower it. Hypertension (high blood pressure) is a major health issue. But it becomes even more frustrating when you are on multiple medications and don’t see any improvements.
People with hard-to-treat, resistant hypertension have a higher risk of stroke, kidney disease and heart failure than people whose high blood pressure is regulated.
If you have resistant hypertension:
- Your blood pressure stays high (reading of 130/80 mmHg and above) — even if you take three blood pressure-lowering medications including one diuretic (water pill).
- You’re taking four or more medications to manage your high blood pressure.
Sometimes an underlying medical condition, or secondary cause, can keep your high blood pressure resistant to medications.
Treating resistant hypertension
Treating resistant hypertension may involve many steps, including:
- Changing blood pressure medicines to find the best combination and dosage.
- Reviewing all your medicines, including those bought without a prescription.
- Checking blood pressure at home to see if medical appointments cause high blood pressure. This is called white coat hypertension.
- Eating healthy, managing weight and making other recommended lifestyle changes.
Subscribe YouTube Channel
- Subscribe Medmichihealthcare YouTube channel
- List of Common Diseases & Medical Disorders
- Buy Complete Premium Anatomy Notes (PDFs)
- Medmichihealthcare New posts
- Read All causes of disease short notes
- Read All diagnosis of disease short notes
- Read All treatment of disease short notes
Discover more from Medmichihealthcare
Subscribe to get the latest posts sent to your email.