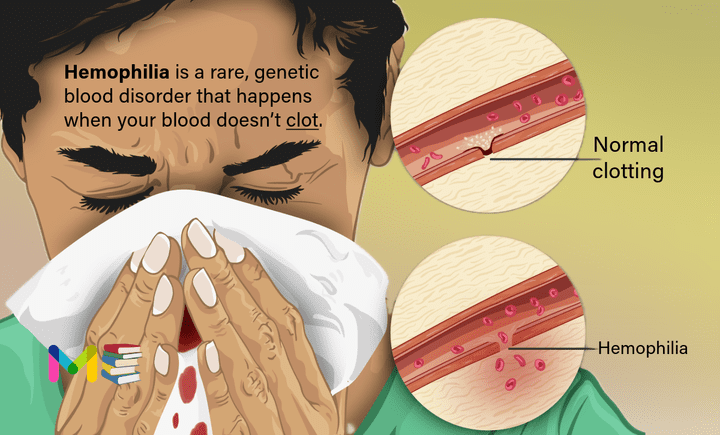
Hemophilia is a rare, genetic blood disorder that happens when your blood doesn’t clot in the typical way and make your bleeding slow down or stop.
People with hemophilia bleed easily because they don’t have enough of one of the clotting factors in their blood. Clotting factors are needed for blood to clot. Blood clots prevent excessive bleeding.
If you have hemophilia, you might bleed for a longer time after an injury than you would if your blood clotted properly.
Small cuts usually aren’t much of a problem. If you have a severe form of the condition, the main concern is bleeding inside your body, especially in your knees, ankles and elbows. Internal bleeding can damage your organs and tissues and be life-threatening.
There are several types of hemophilia. Hemophilia may be severe, moderate or mild based on the amount of clotting factor in your blood.
Healthcare providers treat this condition by replacing the missing clotting factor. There isn’t a cure for hemophilia, but people who receive treatment generally live nearly as long as people who don’t have hemophilia. Providers are researching gene therapy and gene replacement therapy as new ways to treat and possibly cure hemophilia.
Table of Contents
Key points about hemophilia
- Hemophilia is an inherited bleeding disorder. It causes an affected person to have low levels of blood clotting factors.
- The most common symptom of hemophilia is increased, uncontrollable bleeding.
- Treatment with factor VIII or IX can allow a person with hemophilia to manage their disorder well and lead a typical lifestyle.
Types of hemophilia
The three forms of hemophilia include hemophilia A, B, and C.
- Hemophilia A. Type A is the most common type of hemophilia. A deficiency in factor VIII causes this form of hemophilia, which is also known as “classic hemophilia.“
- Hemophilia B. This type of hemophilia, also known as Christmas disease, occurs because clotting factor IX is missing or severely deficient.
- Hemophilia C. Hemophilia C, also known as “factor XI deficiency,“ is a rare form of hemophilia first discovered in 1953 in people with severe bleeding after dental extractions.
Hemophilia is an inherited genetic condition. This condition isn’t curable, but it can be treated to minimize symptoms and prevent future health complications.
Congenital hemophilia
The majority of hemophilia cases are congenital. Congenital means that you acquire the trait from one or both of your parents when you’re born. About two-thirds of all type A and B cases of hemophilia occur in people with a family history of the condition.
Acquired hemophilia
Unlike congenital hemophilia, you can develop acquired hemophilia with no personal or family history of hemophilia. Instead, acquired hemophilia is a rare autoimmune disorder.
An autoimmune disorder or disease occurs when your immune system attacks healthy cells. In the case of acquired hemophilia, the immune system creates antibodies that attack the clotting factors, most frequently factor VIII (acquired hemophilia A).
Symptoms of hemophilia
The most significant symptom is unusual or excessive bleeding or bruising.
- People with hemophilia may develop large bruises after minor injuries. This is a sign of bleeding under their skin.
- They may bleed for an unusually long time, whether that’s bleeding after surgery, bleeding after dental treatment or simply bleeding from a cut finger.
- They may start bleeding for no apparent reason, such as sudden bloody noses.
How much bruising or bleeding people have depends on whether they have severe, moderate or mild hemophilia:
- People with severe hemophilia often have spontaneous bleeding or bleeding for no apparent reason.
- People with moderate hemophilia who have serious injuries may bleed for an unusually long time.
- People with mild hemophilia may have unusual bleeding, but only after major surgery or injury.
Other symptoms may include:
- Joint pain from internal bleeding. Joints in your ankles, knees, hips and shoulders may ache, swell or feel hot to the touch.
- Bleeding into your brain. People with severe hemophilia very rarely develop life-threatening bleeding into their brains. Brain bleeds may cause persistent headaches, double vision or make you feel very sleepy. If you have hemophilia and have these symptoms, get help right away.
Hemophilia symptoms in babies and children
Sometimes, babies assigned male at birth with hemophilia are diagnosed because they bleed more than usual after being circumcised. Other times, children develop symptoms a few months after they’re born. Common symptoms include:
- Bleeding: Babies and toddlers may bleed from their mouths after minor injuries, like bumping their mouths on a toy.
- Swollen lumps on their heads: Babies and toddlers who bump their heads often develop goose eggs, large round lumps on their heads.
- Fussiness, irritability or refusal to crawl or walk: These symptoms may happen if babies and toddlers have internal bleeding into a muscle or joint. They may have areas on their bodies that look bruised and swollen, feel warm to your touch or make your child hurt when you gently touch the area.
- Hematomas: A hematoma is a mass of congealed blood that gathers under babies’ or toddlers’ skin. Babies and toddlers may develop hematomas after receiving an injection.
Types and Symptoms of Diabetes
Causes of hemophilia
When a person bleeds, the body typically pools blood cells together to form a clot to stop the bleeding. Clotting factors are proteins in the blood that work with cells known as platelets to form clots. Hemophilia occurs when a clotting factor is missing or levels of the clotting factor are low.
Congenital hemophilia
Hemophilia is usually inherited, meaning a person is born with the disorder (congenital). Congenital hemophilia is classified by the type of clotting factor that’s low.
The most common type is hemophilia A, associated with a low level of factor 8 The next most common type is hemophilia B, associated with a low level of factor 9.
Acquired hemophilia
Some people develop hemophilia with no family history of the disorder. This is called acquired hemophilia.
Acquired hemophilia is a variety of the condition that occurs when a person’s immune system attacks clotting factor 8 or 9 in the blood. It can be associated with:
- Pregnancy
- Autoimmune conditions
- Cancer
- Multiple sclerosis
- Drug reactions
Hemophilia inheritance
In the most common types of hemophilia, the faulty gene is located on the X chromosome. Everyone has two sex chromosomes, one from each parent. Females inherit an X chromosome from the mother and an X chromosome from the father. Males inherit an X chromosome from the mother and a Y chromosome from the father.
This means that hemophilia almost always occurs in boys and is passed from mother to son through one of the mother’s genes. Most women with the defective gene are carriers who have no signs or symptoms of hemophilia. But some carriers can have bleeding symptoms if their clotting factors are moderately decreased.
Risk factors of hemophilia
The following are the major risk factors of hemophilia:
- Family history. The biggest risk factor for hemophilia is to have family members who also have the disorder. Males are much more likely to have hemophilia than are females.
- Being a male. Hemophilia A and B are more common in people assigned male at birth than people assigned female because the genetic transmission occurs due to a recessive gene on the X chromosome.
- Genetics. Hemophilia C is an autosomal inherited form of the disease, meaning that it affects biological males and biological females equally. This is because the genetic defect that causes this type of hemophilia isn’t related to sex chromosomes.
Causes and Risk Factors of High Blood Pressure
Complications of hemophilia
Complications of hemophilia can include:
- Deep internal bleeding
- Bleeding in the joints or muscles
- Inflammation of the joint lining
- Long-term joint problems
- Development of antibodies (also called inhibitors) against clotting factors
- Pain from joint and muscle bleeds
- Infections from transfusions (HIV and hepatitis B and C). If the clotting factors used to treat hemophilia come from human blood, there’s an increased risk of viral infections such as hepatitis C. Because of donor screening techniques, the risk is low.
Bleeding that occurs in deep muscle can cause the limbs to swell. The swelling can press on nerves and lead to numbness or pain. Depending on where the bleeding occurs, it could be life-threatening. Bleeding into the throat or neck, this can affect a person’s ability to breathe.
Prevention of hemophilia
Hemophilia is a condition that’s typically passed from parent to child. When someone is pregnant, there’s no way of knowing whether the baby has the condition.
However, if your eggs are fertilized in a clinic using in vitro fertilization, they can be tested for the condition. Then, only the eggs without hemophilia can be implanted.
If you’re worried your baby may develop hemophilia, pre-conception and prenatal counseling can help you understand your risk of passing hemophilia on to your baby.
How to manage hemophilia
With careful management and the availability of factor replacement therapy to prevent and treat bleeding, many people with hemophilia can live relatively healthy lives with a normal lifespan.
Managing hemophilia may include:
- Taking part in activities and exercise, but not ones that may cause injury. Talk with the hematologist about which activities are appropriate.
- Getting special care before surgery including dental work. Your healthcare provider may advise factor replacement infusions. These increase clotting levels before the procedures. Specific factor replacement infusions during and after the procedure may also be given. These maintain the clotting factor levels and improve healing and prevention of bleeding after the procedure.
- Preventing dental and gum problems with good dental hygiene.
- Getting vaccines under the skin instead of in the muscle to prevent bleeding in the muscle. If the vaccine must be given in the muscle, using the smallest gauge needle and putting an ice pack on the skin before and soon after can help.
- Avoid aspirin or other nonsteroidal anti-inflammatory drugs (NSAIDs). They increase bleeding risk.
- Wearing medical identification (ID) in the case of an emergency.
Complications and Prevention of High cholesterol
Diagnosis of hemophilia
The diagnosis of hemophilia is based on your family history, your health history, and a physical exam. Blood tests include:
- Complete blood count (CBC). A complete blood count checks the red and white blood cells and platelets (clotting cells). In addition to hemophilia, a low platelet count is another cause of bleeding disorders. Your healthcare provider will want to make sure that your platelet count is normal and that a low platelet count is not the cause of your bleeding.
- Screening tests of clotting times. These are called prothrombin time (PT) and activated partial thromboplastin time (aPTT)
- Mixing studies with certain clotting factors added. This is done to see if the clotting time (aPTT) corrects. This clarifies if there is a deficiency.
- Clotting factors levels (also called factor activity levels). This is a test to check the levels of each clotting factor.
- Genetic or DNA testing. This is done to check for abnormal genes.
Hemophilia is diagnosed through a blood test. Your doctor will remove a small sample of blood from your vein and measure the amount of clotting factor present. The sample is then graded to determine the severity of the factor deficiency and the severity of the condition.
According to National Bleeding Disorders Foundation.
Hemophilia A severity levels include:
- Mild: occurs when factor levels are between 6 and 30 percent (about 25 percent of all cases)
- Moderate: occurs when factor levels are between 1 and 5 percent (about 15 percent of all cases)
- Severe: occurs when factor levels are less than 1 percent (about 60 percent of all cases)
Hemophilia B severity levels include:
- Mild: occurs when factor levels are between 6 and 49 percent
- Moderate: occurs when factor levels are between 1 and 5 percent
- Severe: occurs when factor levels are less than 1 percent
Treatment of hemophilia
The main treatment for severe hemophilia involves replacing the clotting factor you need through a tube in a vein.
This replacement therapy can be given to treat a bleeding episode in progress. It can also be given on a regular schedule at home to help prevent bleeding episodes. Some people receive continuous replacement therapy.
Replacement clotting factor can be made from donated blood. Similar products, called recombinant clotting factors, are made in a laboratory, not from human blood.
Other treatments options based on the type of hemophilia you have, include:
- Clot-preserving medications. Also known as anti-fibrinolytics, these medications help prevent clots from breaking down.
- Concentrated FVIII or FIX product. Often called clotting factor, these infused medications are used to treat types A and B, respectively. The medication can either be synthetic or made from human plasma. Often doctors prescribe them as part of an ongoing, regular treatment regimen known as prophylaxis.
- Aminocaproic acid. This medication helps prevent the breakdown of blood clots. Doctors may prescribe this medication prior to a dental or other procedure.
- Desmopressin. In some forms of mild hemophilia, this hormone can stimulate the body to release more clotting factor. It can be injected slowly into a vein or used as a nasal spray.
- Emicizumab (Hemlibra). This is a newer drug that doesn’t include clotting factors. This drug can help prevent bleeding episodes in people with hemophilia A.
- Fibrin sealants. These can be applied directly to wound sites to promote clotting and healing. Fibrin sealants are especially useful for dental work.
- Physical therapy. It can ease signs and symptoms if internal bleeding has damaged your joints. Severe damage might require surgery.
- First aid for minor cuts. Using pressure and a bandage will generally take care of the bleeding. For small areas of bleeding beneath the skin, use an ice pack. Ice pops can be used to slow down minor bleeding in the mouth.
- Pain management. If you have pain associated with the condition, your doctor may prescribe or recommend pain medications to help alleviate the pain.
Scientists are looking at new forms of therapy, including gene therapies and the use of monoclonal antibodies.
Some people who have replacement therapy develop antibodies, called inhibitors, which attack the clotting factors that control bleeding. Healthcare providers use a technique called immune tolerance induction (ITI). ITI involves clotting factors given on a daily basis to bring down inhibitor levels. ITI may be a long-term treatment, and some people may need this treatment for months or years.
Diagnosis and Treatment of Deep Vein Thrombosis (dvt)
- List of Common Diseases & Medical Disorders
- Buy Complete Premium Anatomy Notes (PDFs)
- Medmichihealthcare New posts
- Read All causes of disease short notes
- Read All diagnosis of disease short notes
- Read All treatment of disease short notes
- Subscribe Medmichihealthcare YouTube channel
Discover more from Medmichihealthcare
Subscribe to get the latest posts sent to your email.