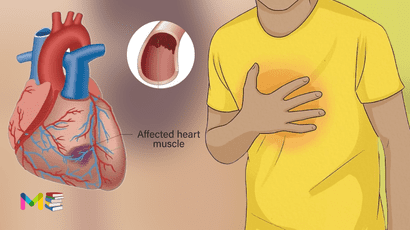
Heart failure also known as congestive heart failure, is a long-term condition in which your heart can’t pump blood well enough to meet your body’s needs.
Your heart is still working. But because it can’t handle the amount of blood it should, blood builds up in other parts of your body. Most of the time, it collects in your lungs, legs and feet.
Certain heart conditions gradually leave the heart too weak or stiff to fill and pump blood properly. These conditions include narrowed arteries in the heart and high blood pressure.
But heart failure can be life-threatening. People with heart failure may have severe symptoms. Some may need a heart transplant or a device to help the heart pump blood.
More than 6 million people in the United States have congestive heart failure. It’s the leading cause of hospitalization in people older than 65.
Proper treatment may improve the symptoms of heart failure and may help some people live longer. Lifestyle changes can improve quality of life. Try to lose weight, exercise, use less salt and manage stress.
Table of Contents
Symptoms of heart failure
Symptoms may develop slowly. Sometimes, heart failure symptoms start suddenly. The symptoms of heart failure may include:
- fatigue
- sudden weight gain
- a loss of appetite
- persistent coughing
- irregular heart rate
- heart palpitations
- abdominal swelling
- shortness of breath
- exercise intolerance
- leg and ankle swelling or abdomen
- sleeping on extra pillows
- getting short of breath while lying down
- protruding neck veins
When to see a healthcare provider
You should see a healthcare provider if you think you might have symptoms of heart failure. Call 911 or emergency medical help if you have any of the following:
- Fainting or severe weakness.
- Chest pain.
- Sudden, severe shortness of breath and coughing up white or pink, foamy mucus.
- Rapid or irregular heartbeat with shortness of breath, chest pain or fainting.
You can also read about symptoms and types of high blood pressure.
Types of heart failure
Heart failure can occur in either the right or left side of your heart. It’s also possible for both sides of your heart to fail at the same time.
Heart failure is also classified as either diastolic or systolic.
- Right-sided heart failure. The right heart ventricle is responsible for pumping blood to your lungs to collect oxygen. Right-sided heart failure occurs when the right side of your heart can’t perform its job effectively. It’s usually triggered by left-sided heart failure. The accumulation of blood in the lungs caused by left-sided heart failure makes the right ventricle work harder. This can stress the right side of the heart and cause it to fail. Right-sided heart failure can also occur because of other conditions, such as lung disease or valve disease. Right-sided heart failure is marked by swelling of the lower extremities or abdomen. This swelling is caused by fluid backup in the legs, feet, and abdomen.
- Left-sided heart failure. Left-sided heart failure is the most common type of heart failure. The left ventricle is located in the bottom left side of your heart. This area pumps oxygen-rich blood to the rest of your body. Left-sided heart failure occurs when the left ventricle doesn’t pump efficiently. This prevents your body from getting enough oxygen-rich blood. The blood backs up into your lungs instead, which causes shortness of breath and a buildup of fluid.
- Diastolic heart failure. Diastolic heart failure occurs when the heart muscle becomes stiffer than normal. The stiffness, which is usually due to heart disease, means that your heart doesn’t fill with blood easily. This is known as diastolic dysfunction. It leads to a lack of blood flow to the rest of the organs in your body. Diastolic heart failure is more common in people who are female than in those who are male.
- Systolic heart failure. Systolic heart failure occurs when the heart muscle loses its ability to contract. The contractions of the heart are necessary to pump oxygen-rich blood out to the body. This problem is known as systolic dysfunction, and it usually develops when your heart is weak and may be enlarged. Systolic heart failure is more common in males than in females. Both diastolic and systolic heart failure can occur on the left or right sides of the heart. You may have either condition on both sides of the heart.
Causes of heart failure
Heart failure can be caused by a weakened, damaged or stiff heart.
- If the main pumping chambers of the heart, called the ventricles, are stiff, they can’t fill with enough blood between beats.
- If the heart is damaged or weakened, the heart chambers may stretch and get bigger. The heart can’t pump out the needed amount of blood.
The heart muscle can be damaged by certain infections, heavy alcohol use, illegal drug use and some chemotherapy medicines. Your genes also can play a role.
Any of the following conditions also can damage or weaken the heart and cause heart failure.
- High blood pressure. Also called hypertension, this condition forces the heart to work harder than it should to pump blood through the body. Over time, the extra work can make the heart muscle too stiff or too weak to properly pump blood.
- Coronary artery disease and heart attack. Coronary artery disease is the most common cause of heart failure. The disease results from the buildup of fatty deposits in the arteries. The deposits narrow the arteries. This reduces blood flow and can lead to heart attack. A heart attack occurs suddenly when an artery feeding the heart becomes completely blocked. Damage to the heart muscle from a heart attack may mean that the heart can no longer pump as well as it should.
- Myocarditis. Myocarditis is most commonly caused by a virus, including the COVID-19 virus, and can lead to left-sided heart failure.
- Heart valve disease. The valves of the heart keep blood flowing the right way. If a valve isn’t working properly, the heart must work harder to pump blood. This can weaken the heart over time. Treating some types of heart valve problems may reverse heart failure.
- Congenital heart defect. If the heart and its chambers or valves haven’t formed correctly, the other parts of the heart have to work harder to pump blood. This may lead to heart failure.
- Arrhythmias. Irregular heart rhythms may cause the heart to beat too fast, creating extra work for the heart. A slow heartbeat also may lead to heart failure. Treating an irregular heart rhythm may reverse heart failure in some people.
- Some long-term diseases may contribute to chronic heart failure. Examples are diabetes, HIV infection, an overactive or underactive thyroid, or a buildup of iron or protein.
Causes of sudden heart failure also include:
- Any illness that affects the whole body.
- Allergic reactions.
- Severe infections.
- Blood clots in the lungs.
- Viruses that attack the heart muscle.
- Use of certain medicines.
Heart failure usually begins with the lower left heart chamber, called the left ventricle. This is the heart’s main pumping chamber. But heart failure also can affect the right side.
The lower right heart chamber is called the right ventricle. Sometimes heart failure affects both sides of the heart.
You can also read about causes and risk factors of stroke.
Risk factors of heart failure
Heart failure can happen to anyone. However, certain factors may increase your risk of developing this condition.
People with diseases that damage the heart are also at an increased risk. These conditions include:
- coronary artery disease
- hypertension
- sleep apnea
- diabetes
- valve disease
- anemia
- hyperthyroidism
- emphysema
- hypothyroidism
Certain lifestyle can also increase your risk of developing heart failure, including:
- having overweight or obesity
- smoking
- not getting enough exercise
- eating foods that are high in fat or cholesterol
Medications that may increase risk of heart failure include:
- Some medication used for diabetes . The diabetes drugs rosiglitazone (Avandia) and pioglitazone (Actos) have been found to increase the risk of heart failure in some people. Don’t stop taking these medicines without first talking to your health care provider.
- Some other medications. Other medications that may lead to heart failure or heart problems include nonsteroidal anti-inflammatory drugs (NSAIDs) and some medicines used to treat high blood pressure, cancer, blood conditions, irregular heartbeats, nervous system diseases, mental health conditions, lung and urinary problems, and infections.
You can also read about risk factors and complications of diabetes.
Complications of heart failure
Complications of heart failure depend on your age, overall health and the severity of heart disease. They may include:
- Irregular heartbeat.
- Sudden cardiac arrest.
- Heart valve problems.
- A collection of fluid in your lungs.
- Pulmonary hypertension.
- Kidney damage.
- Liver damage.
- Malnutrition.
Prevention of heart failure
Some lifestyle measures can help treat heart failure and prevent the condition from developing.
Maintaining a moderate weight and exercising regularly can significantly decrease your risk of heart failure. Reducing the amount of salt in your diet can also lower your risk.
Other habits that may prevent heart failure include:
- not smoking
- limiting alcohol intake
- avoiding high fat foods
- staying active
- getting the right amount of sleep
Diagnosis of heart failure
To properly diagnose heart failure, your health care provider examines you and asks questions about your symptoms and medical history. Your provider checks to see if you have risk factors for heart failure, such as high blood pressure, coronary artery disease or diabetes.
Your care provider listens to your lungs and heart with a device called a stethoscope. A whooshing sound called a murmur may be heard when listening to your heart. Your provider may look at the veins in your neck and check for swelling in your legs and belly.
Tests used for heart failure
- Chest X-ray. X-ray images can show the condition of the lungs and heart.
- Blood tests. Blood tests can help diagnose diseases that can affect the heart. Blood tests also can look for a specific protein made by the heart and blood vessels. In heart failure, the level of this protein goes up.
- Electrocardiogram (ECG or EKG). This quick and painless test records the electrical signals in the heart. It can show how fast or how slowly the heart is beating.
- Echocardiogram. Sound waves create images of the beating heart. This test shows the size and structure of the heart and heart valves and blood flow through the heart.
- Ejection fraction. Ejection fraction is a measurement of the percentage of blood leaving your heart each time it squeezes. This measurement is taken during an echocardiogram. The result helps classify heart failure and guides treatment. An ejection fraction of 50% or higher is considered ideal. But you can still have heart failure even if the number is considered ideal.
- CT scan of the heart. Also called a cardiac CT scan, this test uses X-rays to create cross-sectional images of the heart.
- Heart MRI scan (Cardiac MRI). This test uses magnetic fields and radio waves to create detailed images of the heart.
- Coronary angiogram. This test helps spot blockages in the heart arteries. The health care provider inserts a long, thin flexible tube called a catheter into a blood vessel, usually in the groin or wrist. It’s then guided to the heart. Dye flows through the catheter to arteries in the heart. The dye helps the arteries show up more clearly on X-ray images and video.
- Myocardial biopsy. In this test, a health care provider removes very small pieces of the heart muscle for examination. This test may be done to diagnose certain types of heart muscle diseases that cause heart failure.
- Exercise tests or stress tests. These tests often involve walking on a treadmill or riding a stationary bike while the heart is monitored. Exercise tests can show how the heart responds to physical activity. If you can’t exercise, you might be given medicines.
During or after testing for heart failure, your health care provider may tell you the stage of disease. Staging helps determine the most appropriate treatment.
According to New York Heart Association (NYHA) classification
This system groups heart failure into four categories by number. You may see Roman numerals used for these category names.
- Class 1 heart failure. There are no heart failure symptoms.
- Class 2 heart failure. Everyday activities can be done without difficulty. But exertion causes shortness of breath or fatigue.
- Class 3 heart failure. It’s difficult to complete everyday activities.
- Class 4 heart failure. Shortness of breath occurs even at rest. This category includes the most severe heart failure.
According to American College of Cardiology/American Heart Association classification
This stage-based classification system uses letters A to D. It includes a category for people who are at risk of developing heart failure.
- Stage A. There are several risk factors for heart failure but no signs or symptoms.
- Stage B. There is heart disease but no signs or symptoms of heart failure.
- Stage C. There is heart disease and signs or symptoms of heart failure.
- Stage D. Advanced heart failure requires specialized treatments.
Health professionals often use the classification systems together to help decide the most appropriate treatment options. Your provider can help you interpret your stage.
Treatment of heart failure
Treatment of heart failure will depend on the type of heart failure you have and, in part, what caused it. Medications and lifestyle changes are part of every heart failure treatment plan. Your healthcare provider will talk to you about the best treatment plan for you.
There’s no cure for heart failure. As congestive heart failure gets worse, your heart muscle pumps less blood to your organs, and you move toward the next stage of heart failure. Since you can’t move backward through the heart failure stages, the goal of treatment is to keep you from moving forward through the stages or to slow down the progression of your heart failure.
Treatment for stage A heart failure
The treatments includes:
- Treatment for high blood pressure (medication, low-sodium diet, active lifestyle).
- Regular exercise, such as walking every day.
- Treatment for high cholesterol.
- Angiotensin-converting enzyme inhibitor (ACE-I) or an angiotensin II receptor blocker (ARB) if you have coronary artery disease, diabetes, high blood pressure or other vascular or cardiac conditions.
- No tobacco products.
- No alcohol or recreational drugs.
Treatment for stage B heart failure
Treatments include:
- Treatments for Stage A.
- Angiotensin-converting enzyme inhibitor (ACE-I) or angiotensin II receptor blocker (ARB) if your EF is 40% or lower.
- Aldosterone antagonist if you’ve had a heart attack or if you have an EF of 35% or less.
- Beta-blocker if you’ve had a heart attack and your EF is 40% or lower (if you aren’t already taking one).
- Possible surgery or intervention as a treatment for coronary artery blockage, heart attack, valve disease (valve repair or replacement) or congenital heart disease.
Treatment for stage C heart failure
Treatments include:
- Treatments from Stages A and B.
- Aldosterone antagonist.
- Beta-blocker.
- Sodium-glucose transport 2 inhibitors (SGLT2i).
- Hydralazine/nitrate combination if other treatments don’t stop your symptoms and you’re African American.
- Medications that slow your heart rate if your heart rate is faster than 70 beats per minute and you still have symptoms.
- A diuretic (“water pill”) if symptoms continue.
- Restriction of sodium (salt) in your diet.
- Weight tracking every day. Tell your healthcare provider if you gain or lose more than 4 pounds.
- Possible cardiac resynchronization therapy (biventricular pacemaker).
- Possible implantable cardiac defibrillator (ICD) therapy.
- Possible fluid restriction.
If the treatment improves or stops your symptoms, you still need to continue treatment to slow the progression to Stage D.
Treatment for stage D heart failure
Treatments include:
Treatment for people who have Stage D heart failure includes treatments for Stages A, B and C. In addition, it includes evaluation for more advanced treatment options, including:
- Heart transplant.
- Ventricular assist devices.
- Heart surgery.
- Continuous infusion of inotropic drugs.
- Palliative or hospice care.
Stages C and D with preserved EF
Treatment for people with Stage C and Stage D heart failure and preserved EF (HFpEF) includes:
- Treatments for Stages A and B.
- Diuretic (“water pill”) to reduce or relieve symptoms.
- Medications for the treatment of medical conditions that can cause heart failure or make it worse, such as atrial fibrillation, high blood pressure, diabetes, obesity, coronary artery disease, chronic lung disease, high cholesterol and kidney disease.
It’s very important for you to manage other underlying conditions, such as:
- High blood pressure.
- Diabetes.
- Kidney disease.
- Anemia.
- Asthma.
- Chronic lung disease.
- Thyroid disease.
Some conditions have signs and symptoms similar to heart failure. If you have new or worsening nonurgent symptoms, tell your healthcare provider.
People with congestive heart failure may need to limit how much salt and/or fluid they consume each day.
Congestive heart failure is a chronic, long-term illness that can get worse quickly, so it’s a good idea to let your provider and family know your preferences for medical care.
It’s important to recognize that heart failure can happen to anyone. It’s important to take lifelong preventive measures for your heart health. Always contact your doctor if you suddenly have any new or unexplained symptoms that may indicate a problem with your heart.
Subscribe YouTube Channel
- Subscribe Medmichihealthcare YouTube channel
- List of Common Diseases & Medical Disorders
- Buy Complete Premium Anatomy Notes (PDFs)
- Medmichihealthcare New posts
- Read All causes of disease short notes
- Read All diagnosis of disease short notes
- Read All treatment of disease short notes
Discover more from Medmichihealthcare
Subscribe to get the latest posts sent to your email.