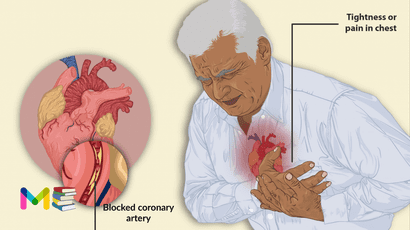
Heart attack (myocardial infarction) is a very dangerous condition that occur because of a lack of blood flow to your heart muscle. The lack of blood flow can occur because of many different factors but is usually related to a blockage in one or more of your heart’s arteries.
Without blood flow, the affected heart muscle will begin to die. If blood flow isn’t restored quickly, it can cause permanent heart damage and death. The blockage is usually due to a buildup of fat, cholesterol and other substances in the heart (coronary) arteries. The fatty, cholesterol-containing deposits are called plaques. The process of plaque buildup is known as atherosclerosis.
Sometimes, a plaque can rupture and form a clot that blocks blood flow. A lack of blood flow can damage or destroy part of the heart.
If you, or someone around you, experiences the symptoms of a heart attack, call emergency services or 911 immediately.
While most people who have a heart attack survive, it’s important to know how how to reduce your risk and how to respond if you experience symptoms of a heart attack.
Table of Contents
Symptoms of heart attacks
Symptoms vary depending on how mild or severe it is, and some people may even have no symptoms at all.
Common symptoms include the following:
- Pain or discomfort that spreads to the shoulder, arm, back, neck, jaw, teeth or sometimes the upper belly
- Chest pain that may feel like pressure, tightness, pain, squeezing or aching
- Cold sweat
- Fatigue
- Heartburn or indigestion
- Lightheadedness or sudden dizziness
- Shortness of breath
- Nausea
Women may have atypical symptoms which can include:
- brief or sharp pain felt in the neck, arm or back.
- Sometimes, the first symptom sign of a heart attack is sudden cardiac arrest.
Some heart attacks strike suddenly. But many people have warning signs and symptoms hours, days or weeks in advance.
Chest pain or pressure (angina) that keeps happening and doesn’t go away with rest may be an early warning sign. Angina is caused by a temporary decrease in blood flow to the heart.
You can also read about types and symptoms of heart failure.
Types of heart attack
Heart attacks can be classified by partial or complete blockage of the heart (coronary) artery.
- A partial blockage often means you’ve had a non-ST elevation myocardial infarction (NSTEMI). However, some people with non-ST elevation myocardial infarction (NSTEMI) have a total blockage.
- An acute complete blockage of a medium or large heart artery usually means you’ve had an ST elevation myocardial infarction (STEMI).
- Other heart attack conditions are not caused by blockage. it can be rare medical conditions, spasm, trauma, electrolyte imbalance and more.
What to do if you have a heart attack
The first thing to do if you notice you are having a heart attack, is to get help or seek medical emergency immediately. You can take the following steps:
- Call for emergency medical help. If you think you’re having a heart attack, immediately call 911 or your local emergency number. If you don’t have access to emergency medical services, have someone drive you to the nearest hospital. Drive yourself only if there are no other options.
- Take nitroglycerin, if prescribed to you by a health care provider. Take it as instructed while awaiting emergency help.
- Take aspirin, if recommended. Taking aspirin during a heart attack may reduce heart damage by preventing blood clotting. Aspirin can interact with other drugs. Don’t take an aspirin unless your care provider or emergency medical personnel say to do so. Don’t delay calling 911 to take an aspirin. Call for emergency help first.
How to help someone having a heart attack
If you are with someone who’s experiencing symptoms of a heart attack, call emergency services immediately and follow the instructions they give you regarding what to do.
If the person isn’t responsive and doesn’t have a pulse, doing cardiopulmonary resuscitation (CPR) or using an automated external defibrillator (AED) can be lifesaving.
Most businesses and many public places have AEDs, but if one isn’t present, CPR shouldn’t be delayed. Giving CPR can help pump oxygenated blood through a person’s body until emergency services arrive.
The sooner a person can get emergency medical attention, the less damage their heart muscle will likely sustain.
You can also read about symptoms and causes of stroke.
Causes of heart attacks
The vast majority of heart attacks occur because of a blockage in one of the blood vessels that supplies the heart. This most often happens because of plaque, a sticky substance that can build up on the insides of your arteries. That buildup is called atherosclerosis.
Sometimes, the plaque deposits inside the coronary (heart) arteries can break open or rupture, and a blood clot can get stuck where the rupture occur. If the clot blocks the artery, this can deprive the heart muscle of blood and cause heart attacks.
This condition is possible without a blockage, but this is rare and only accounts for about 5% of all heart attacks. This kind of heart attack can occur for the following reasons:
- Rare medical conditions: An example of this would be any disease that causes unusual narrowing of blood vessels.
- Coronary artery spasm.
- Trauma: This includes tears or ruptures in the coronary arteries.
- Obstruction that came from somewhere else in your body: A blood clot or air bubble (embolism) that gets trapped in a coronary artery.
- Electrolyte imbalance.
- Takotsubo or stress cardiomyopathy.
- Anomalous coronary arteries (a congenital heart defect you’re born with where the coronary arteries are in different positions than normal in your body. Compression of these causes a heart attack).
- Eating disorders: Over time, these can damage your heart and ultimately result in a heart attack.
Risk factors of heart attacks
The following are the risk factors of heart attacks, this include:
- High blood pressure. Over time, high blood pressure can damage arteries that lead to the heart. High blood pressure that occurs with other conditions, such as obesity, high cholesterol or diabetes, increases the risk even more.
- High cholesterol or triglycerides. A high level of low-density lipoprotein (LDL) cholesterol (the “bad” cholesterol) is most likely to narrow arteries. A high level of certain blood fats called triglycerides also increases heart attack risk. Your heart attack risk may drop if levels of high-density lipoprotein (HDL) cholesterol, the “good” cholesterol are in the standard range.
- Diabetes. Blood sugar rises when the body doesn’t make a hormone called insulin or can’t use it correctly. High blood sugar increases the risk of a heart attack.
- Age. Men age 45 and older and women age 55 and older are more likely to have a heart attack than are younger men and women.
- Tobacco use. This includes smoking and long-term exposure to secondhand smoke. If you smoke, quit.
- Obesity. Obesity is linked with high blood pressure, diabetes, high levels of triglycerides and bad cholesterol, and low levels of good cholesterol.
- Metabolic syndrome. This is a combination of at least three of the following things: enlarged waist (central obesity), high blood pressure, low good cholesterol, high triglycerides and high blood sugar. Having metabolic syndrome makes you twice as likely to develop heart disease than if you don’t have it.
- Family history of heart attacks. If a brother, sister, parent or grandparent had an early heart attack (by age 55 for males and by age 65 for females), you might be at increased risk.
- Not enough exercise. A lack of physical activity (sedentary lifestyle) is linked to a higher risk of heart attacks. Regular exercise improves heart health.
- Unhealthy diet. A diet high in sugars, animal fats, processed foods, trans fats and salt increases the risk of heart attacks. Eat plenty of fruits, vegetables, fiber and healthy oils.
- Stress. Emotional stress, such as extreme anger, may increase the risk of a heart attack.
- A history of preeclampsia. This condition causes high blood pressure during pregnancy. It increases the lifetime risk of heart disease.
- An autoimmune condition. Having a condition such as rheumatoid arthritis or lupus can increase the risk of a heart attack.
- Illegal drug use. Cocaine and amphetamines are stimulants. They can trigger a coronary artery spasm that can cause a heart attack.
You can also read about risk factors and complications of diabetes.
Complications of heart attacks
The complications of heart attack is due to damage to the heart muscle. Some of the complications of heart attacks include:
- Irregular or atypical heart rhythms (arrhythmias). Heart attack damage can affect how electrical signals move through the heart, causing heartbeat changes. Some may be serious and can be deadly.
- Cardiogenic shock. This rare condition occurs when the heart is suddenly and abruptly unable to pump blood.
- Cardiac arrest. Without warning, the heart stops. A sudden change in the heart’s signaling causes sudden cardiac arrest. A heart attack increases the risk of this life-threatening condition. It can lead to death (sudden cardiac death) without immediate treatment.
- Heart failure. A lot of damage to the heart muscle tissue can make the heart unable to pump blood. Heart failure can be temporary or long-lasting (chronic).
- Inflammation of the saclike tissue surrounding the heart (pericarditis). Sometimes a heart attack triggers a faulty immune system response. This condition may be called Dressler syndrome, postmyocardial infarction syndrome or postcardiac injury syndrome.
Prevention of heart attacks
There are many risk factors of heart attacks that you cannot control, but there are some basic steps you can take to help keep a healthy heart. The following are few examples:
- Work with your doctor. If you have a heart condition, work closely with your doctor and follow your treatment plan, which includes taking your medications.
- Exercise regularly. Try to get at least 150 minutes of physical activity a week for optimum heart health.
- Eat a healthy, balanced diet. Try to incorporate nutrient-rich foods in your diet as often as possible. Focus on lean proteins, whole grains, fruit, vegetables, low-fat dairy, nuts, and seeds. Try to limit fatty, fried foods and foods that contain simple sugars like sodas, baked goods, and white bread.
- Get your cholesterol levels checked. If your LDL cholesterol or triglycerides are higher than they should be, talk with your doctor about what you need to do to lower your cholesterol and triglycerides.
- Manage diabetes. If you have diabetes, take your medications as your doctor prescribed and check your blood glucose levels regularly.
- Quit smoking. If you smoke, consider talking with your doctor about starting a smoking cessation program. Quitting smoking can help reduce your risk because smoking is a major cause of heart disease.
- Limit your alcohol intake. Moderation is key when it comes to alcohol and heart health. Light to moderate alcohol consumption is defined as one drink per day for women and two drinks per day for men.
The above steps are very important in lowering your risk of developing heart disease and potentially having heart attacks. Talk with your doctor if you have concerns about your risk of having the condition.
You can also read about prevention and diagnosis of myocarditis.
Diagnosis of heart attacks
The first thing your provider will do is to perform a physical exam, including checking pulse, blood oxygen levels, blood pressure and listening to heart and lung sounds. Also will review your medical history.
The following are the test required to diagnose heart attacks, which include:
- History and symptoms. The provider will ask you about the symptoms you experienced. They might also ask someone who was with you to describe what happened.
- Blood tests. During a heart attack, the damage to heart muscle cells almost always causes a chemical marker, a cardiac troponin, to appear in your bloodstream. Blood tests that look for that marker are among the most reliable methods to diagnose a heart attack.
- Electrocardiogram (EKG or ECG). This is one of the first tests you get when you come to an ER with heart attack symptoms.
- Echocardiogram. Using ultrasound (high-frequency sound waves), an echocardiogram generates a picture of the inside and outside of your heart.
- Angiogram. This test shows areas with little or no blood flow.
- Heart computed tomography (CT) scan. This creates a highly detailed scan of your heart.
- Heart MRI. This test uses a powerful magnetic field and computer processing to create an image of your heart.
- Nuclear heart scans. Similar to angiography, these scans use a radioactive dye injected into your blood. What sets them apart from an angiogram is that they use computer-enhanced methods like computed tomography (CT) or positron emission tomography (PET) scans.
Treatment of heart attacks
The time of getting treatment is crucial with a heart attack patient. The sooner you get treatment after having a heart attack, the better quickly blood flow can be restored to the affected part of your heart muscle, and the more successful likely the result.
Urgent treatment is needed to fix blood flow and restore oxygen levels. Oxygen is given immediately. Specific heart attack treatment depends on whether there’s a partial or complete blockage of blood flow.
Treatment may include medications and surgical/nonsurgical procedures:.
Heart attack medication
Medicines to treat heart attacks include:
- Clot busters (thrombolytics or fibrinolytics). These drugs help break up any blood clots that are blocking blood flow to the heart. The earlier a thrombolytic drug is given after a heart attack, the less the heart is damaged and the greater the chance of survival.
- Aspirin. Aspirin reduces blood clotting. It helps keep blood moving through a narrowed artery. If you called 911 or your local emergency number, you may be told to chew aspirin. Emergency medical providers may give you aspirin immediately.
- Other blood-thinning medications. A medicine called heparin may be given by or injection. Heparin makes the blood less sticky and less likely to form clots.
- Nitroglycerin. This medication widens the blood vessels. It helps improve blood flow to the heart. Nitroglycerin is used to treat sudden chest pain (angina). It’s given as a pill under the tongue, as a pill to swallow or as an injection.
- Beta blockers. These medications slow the heartbeat and decrease blood pressure. Beta blockers can limit the amount of heart muscle damage and prevent future heart attacks. They are given to most people who are having a heart attack.
- angiotensin-converting enzyme (ACE) inhibitors. These drugs lower blood pressure and reduce stress on the heart.
- Statins. These drugs help lower unhealthy cholesterol levels. Too much bad (low-density lipoprotein, or LDL) cholesterol can clog arteries.
- Morphine. This medicine is given to relieve chest pain that doesn’t go away with nitroglycerin.
Surgical and nonsurgical procedures
If you’ve had a heart attack, your provider may recommend some procedures (surgical or nonsurgical). These will relieve pain and help prevent another one from happening.
This procedures may include:
- Coronary artery bypass surgery (CABG). This is open-heart surgery. A surgeon takes a healthy blood vessel from another part of the body to create a new path for blood in the heart. The blood then goes around the blocked or narrowed coronary artery. coronary artery bypass surgery (CABG) may be done as an emergency surgery at the time of a heart attack. Sometimes it’s done a few days later, after the heart has recovered a bit.
- Coronary angioplasty and stenting. This procedure is done to open clogged heart arteries. It may also be called percutaneous coronary intervention (PCI). If you’ve had a heart attack, this procedure is often done during a procedure to find blockages (cardiac catheterization).During angioplasty, a heart doctor (cardiologist) guides a thin, flexible tube (catheter) to the narrowed part of the heart artery. A tiny balloon is inflated to help widen the blocked artery and improve blood flow.A small wire mesh tube (stent) may be placed in the artery during angioplasty. The stent helps keep the artery open. It lowers the risk of the artery narrowing again. Some stents are coated with a medication that helps keep the arteries open.
- Heart valve surgery. In valve repair or replacement surgery, surgeons repair or replace leaky valves to help the heart pump.
- Pacemaker. A pacemaker is a device implanted beneath the skin. It can help your heart maintain a normal rhythm.
- Heart transplant. Surgeons may recommend a heart transplant in cases where a heart attack causes permanent tissue death to most of the heart.
Cardiac rehabilitation is a personalized exercise and education program that teaches ways to improve heart health after heart surgery. It focuses on exercise, a heart-healthy diet, stress management and a gradual return to usual activities.
Most hospitals offer cardiac rehabilitation starting in the hospital. The program typically continues for a few weeks or months after you return home.
People who attend cardiac rehab after a heart attack generally live longer and are less likely to have another heart attack or complications from the heart attack. If cardiac rehab is not recommended during your hospital stay, ask your provider about it.
Subscribe YouTube Channel
- Subscribe Medmichihealthcare YouTube channel
- List of Common Diseases & Medical Disorders
- Buy Complete Premium Anatomy Notes (PDFs)
- Medmichihealthcare New posts
- Read All causes of disease short notes
- Read All diagnosis of disease short notes
- Read All treatment of disease short notes
Discover more from Medmichihealthcare
Subscribe to get the latest posts sent to your email.