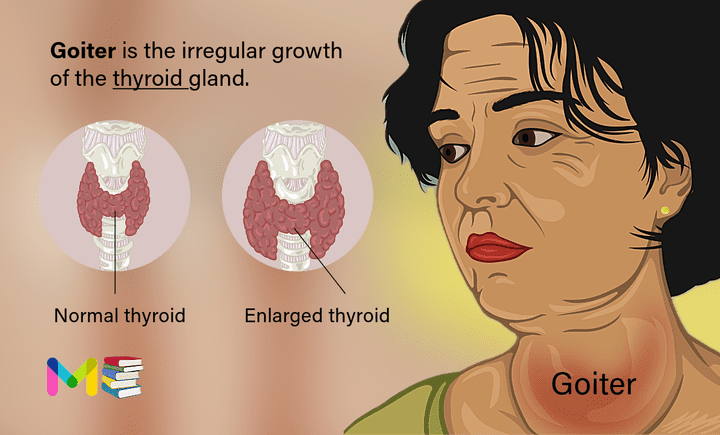
A goiter is the irregular growth of the thyroid gland. Your entire thyroid can grow larger or it can develop one or more small lumps called thyroid nodules.
The thyroid is a butterfly-shaped gland located at the base of the neck just below the Adam’s apple. It produces the hormones thyroxine (also called T4) and triiodothyronine (also called T3). These hormones play a role in certain bodily functions, including:
- Metabolism.
- Body temperature.
- Mood and excitability.
- Pulse and heart rate.
- Digestion.
- Other hormone interactions
The thyroid gland also produces calcitonin, a hormone that helps regulate the amount of calcium in the blood.
The pituitary gland and the hypothalamus are located within the brain and control hormone production. The pituitary gland and hypothalamus control the rate at which T-4 and T-3 are produced and released.
The hypothalamus is a specialized region at the base of the brain. It acts as a thermostat for maintaining balance in multiple body systems. The hypothalamus signals the pituitary gland to make a hormone known as thyroid-stimulating hormone (TSH).
The pituitary gland — located below the hypothalamus — releases a certain amount of thyroid-stimulating hormone (TSH), depending on how much T-4 and T-3 are in the blood. The thyroid gland, in turn, regulates its production of hormones based on the amount of TSH it receives from the pituitary gland.
Goiter may be associated with an irregular amount of thyroid hormone in your body (hypothyroidism or hyperthyroidism) or with normal levels of thyroid hormone (euthyroid). Goiter has several possible causes and may develop in anyone, but is more common in women. Your risk of developing goiter also increases as you age. They’re more common after age 40.
Widespread enlargement of the thyroid can expand the gland well beyond its typical size (left) and cause a noticeable bulge in the neck (right). The most common cause of goiters worldwide is a lack of iodine in the diet.
Treatment depends on the cause of the goiter, symptoms, and complications resulting from the goiter. Small goiters that aren’t noticeable and don’t cause problems usually don’t need treatment.
Table of Contents
Key points about goiter
- Goiter is an enlarged thyroid gland. Your thyroid is the butterfly-shaped gland at the base of your neck.
- Goiter can show as an obvious lump or swelling at the bottom of your neck. Goiters are usually painless but can feel sore or tender. A large goiter can make it hard to breathe or swallow.
- Goiter can also affect the amount of thyroid hormone that you make.
- There are several causes, and your treatment will depend on the cause of your goiter.
Types of goiter
Goiter can be classified in a few different ways, including the way by which it grows and if your thyroid hormone levels are irregular or not.
Classifications for goiter based on how it enlarges include:
- Colloid goiter. A colloid goiter develops from the lack of iodine, a mineral essential to the production of thyroid hormones. People who get this type of goiter usually live in areas where iodine is scarce.
- Simple (diffuse) goiter: This type of goiter happens when your entire thyroid gland swells and feels smooth to the touch.
- Nodular goiter: This type of goiter happens when a solid or fluid-filled lump called a nodule develops within your thyroid and makes it feel lumpy.
- Multinodular goiter: This type of goiter happens when there are many lumps (nodules) within your thyroid. The nodules may be visible or only discovered through examination or scans.
Classifications of goiter based on thyroid hormone levels include:
- Toxic goiter: This goiter happens when your thyroid is enlarged and produces too much thyroid hormone.
- Nontoxic goiter: If you have an enlarged thyroid but normal thyroid levels (euthyroid), it’s a nontoxic goiter. In other words, you don’t have hyperthyroidism (overactive thyroid) or hypothyroidism (underactive thyroid).
Healthcare providers combine these descriptors to classify certain types of goiter when diagnosing them. For example, a toxic multinodular goiter happens when there’s more than one nodule on your thyroid — usually several — producing an extra amount of thyroid hormone.
Symptoms of goiter
Most people with goiters have no signs or symptoms other than a swelling at the base of the neck. In many cases, the goiter is small enough that it’s only discovered during a routine medical exam or an imaging test for another condition. Most goiters are painless, but if you have thyroiditis (an inflamed thyroid gland), it can be painful. The main symptoms of goiter include:
- A lump in the front of your neck, just below your Adam’s apple.
- A feeling of tightness in your throat area.
- Hoarseness (scratchy voice).
- Neck vein swelling.
- Dizziness when you raise your arms above your head.
Other, less common symptoms include:
- Difficulty breathing (shortness of breath).
- Coughing.
- Wheezing (due to squeezing of your windpipe).
- Difficulty swallowing (due to squeezing of your esophagus).
Some people who have a goiter may also have hyperthyroidism (overactive thyroid), hypothyroidism (underactive thyroid), and Obstructive goiter.
Signs and Symptoms of hyperthyroidism (Overactive thyroid)
- Weight loss
- Rapid heartbeat (tachycardia)
- Increased sensitivity to heat
- Excess sweating
- Tremors
- Irritability and nervousness
- Muscle weakness
- Frequent bowel movements
- Changes in menstrual patterns
- Sleep difficulty
- High blood pressure
- Increased appetite
Children with hyperthyroidism might also have the following:
- Rapid growth in height
- Changes in behavior
- Bone growth that outpaces expected growth for the child’s age
Signs and Symptoms of hypothyroidism (Underactive thyroid)
- Fatigue
- Increased sensitivity to cold
- Increased sleepiness
- Dry skin
- Constipation
- Muscle weakness
- Problems with memory or concentration
Signs and Symptoms of Obstructive goiter
The size or position of a goiter may obstruct the airway and voice box. Signs and symptoms may include:
- Difficulty swallowing
- Difficulty breathing with exertion
- Cough
- Hoarseness
- Snoring
Causes of goiter
Goiter is an adaptive reaction of the cells in your thyroid to any process that blocks thyroid hormone production. A number of factors that influence thyroid function or growth can result in a goiter. While the most common cause of goiter worldwide is iodine deficiency, many conditions can cause it.
Causes of goiter include:
- Iodine deficiency. Iodine is essential for the production of thyroid hormones. If a person does not get enough dietary iodine, hormone production drops and the pituitary gland signals the thyroid to make more. This increased signal results in thyroid growth.
- Hashimoto’s disease. Hashimoto’s disease is an autoimmune disorder, an illness caused by the immune system attacking healthy tissues. The damaged and inflamed tissues of the thyroid don’t produce enough hormones (hypothyroidism). When the pituitary gland detects the decline and prompts the thyroid to create more hormones, the thyroid can become enlarged.
- Graves’ disease. Another autoimmune disorder called Graves’ disease occurs when the immune system produces a protein that mimics TSH. This rogue protein prompts the thyroid to overproduce hormones (hyperthyroidism) and can result in thyroid growth.
- Thyroid nodules. A nodule is the irregular growth of thyroid cells that form a lump. A person may have one nodule or several nodules (multinodular goiter). The cause of nodules is not clear, but there may be multiple factors — genetics, diet, lifestyle and environment. Most thyroid nodules are noncancerous (benign).
- Thyroid cancer. Thyroid cancer is less common than other cancers and generally treatable. About 5% of people with thyroid nodules are found to have cancer.
- Pregnancy. A hormone produced during pregnancy, human chorionic gonadotropin (HCG), may cause the thyroid gland to be overactive and enlarge slightly.
- Thyroiditis. Inflammation of the thyroid caused by an autoimmune disorder, bacterial or viral infection, or medication. The inflammation may cause hyperthyroidism or hypothyroidism.
Nontoxic goiter (sporadic). In most cases, have no known cause. In some cases, certain drugs can cause this type of goiter. For example, the drug lithium, which is used to treat certain mental health conditions, as well as other medical conditions, can cause this type of goiter.
The more severe the iodine deficiency, the more likely someone is to have goiter:
- With mild iodine deficiency, the incidence of goiter is 5% to 20%.
- With a moderate iodine deficiency, the prevalence increases to 20% to 30%.
- With severe iodine deficiency, the incidence increases to greater than 30%.
Risk factors of goiter
Anyone can develop a goiter. It may be present at birth or occur at any time throughout life. Some common risk factors for goiters include:
- A lack of dietary iodine. Iodine is found primarily in seawater and in the soil in coastal areas. In the developing world in particular, people who don’t have enough iodine in their diets or access to food supplemented with iodine are at increased risk.
- Being female. Women are more likely to develop a goiter or other thyroid disorders.
- Pregnancy and menopause. Thyroid problems in women are more likely to occur during pregnancy and menopause.
- Age. Goiters are more common after age 40.
- Family medical history. Family medical history of goiters or other thyroid disorders increases the risk of goiters. Also, researchers have identified genetic factors that may be associated with an increased risk.
- Medications. Some medical treatments, including the heart drug amiodarone (Pacerone) and the psychiatric drug lithium (Lithobid), increase your risk.
- Radiation exposure. Your risk increases if you’ve had radiation treatments to your neck or chest area.
People who have any of the following conditions may also be more likely to develop goiter:
- Obesity.
- Insulin resistance.
- Metabolic syndrome.
Causes and risk factors of Sleep apnea
Complications of goiter
A goiter itself usually doesn’t cause complications. The appearance may be troublesome or embarrassing for some people. A large goiter may obstruct the airway and voice box.
Changes in the production of thyroid hormones that may be associated with goiters have the potential for causing complications in multiple body systems.
Prevention of goiter
A goiter caused by iodine deficiency (simple goiter) is generally the only type of goiter you can prevent. Consuming a diet that includes fish, dairy and a healthy amount of iodized table salt prevents these types of goiters. Iodine supplements and other supplements are generally not recommended and may do more harm than good.
Complications and prevention of Sinusitis
Diagnosis of goiter
A goiter is often discovered during a routine physical exam. By touching your neck, your health care provider may detect an enlargement of the thyroid, an individual nodule or multiple nodules. Sometimes a goiter is found when you are undergoing an imaging test for another condition. Additional tests are then ordered to do the following:
- Measure the size of the thyroid
- Detect any nodules
- Assess whether the thyroid may be overactive or underactive
- Determine the cause of the goiter
Several tests to diagnose and evaluate goiter include:
- Physical exam: Your provider may be able to tell if your thyroid gland is enlarged by feeling your neck area for nodules and signs of tenderness.
- Thyroid blood test: This blood test measures thyroid hormone levels, which reveal if your thyroid is working properly.
- Antibody test: This blood test looks for certain antibodies that are produced in some forms of goiter. An antibody is a protein made by white blood cells. Antibodies help defend against invaders (for example, viruses) that cause disease or infection in your body.
- Thyroid ultrasound or Ultrasonography: Ultrasound is a procedure that sends high-frequency sound waves through body tissues. The echoes are recorded and transformed into video or photos. Your provider can “see” your thyroid to check its size and if it has nodules.
- Biopsy: A biopsy is the removal of a sample of tissue or cells to be studied in a laboratory. You may need a thyroid biopsy if there are large nodules in your thyroid gland. A biopsy is taken to rule out cancer.
- Thyroid uptake and scan or Radioactive iodine intake: This imaging test provides information on the size and function of your thyroid. In this test, a small amount of radioactive material is injected into a vein to produce an image of your thyroid on a computer screen. Providers don’t order this test very often, since it’s only useful in certain circumstances.
- CT scan or MRI (magnetic resonance imaging) of your thyroid: If the goiter is very large or spreads into your chest, a CT scan or MRI is used to measure the size and spread of the goiter.
Treatment of goiter
A simple goiter may happen for only a short time and may go away on its own without treatment. Many goiters, such as multinodular goiter, are associated with normal levels of thyroid hormone. These goiters usually don’t require any specific treatment after your healthcare provider has diagnosed it. However, you may be at risk of developing hypothyroidism or hyperthyroidism in the future.
If you have an enlarged thyroid gland, it’s still important to see your healthcare provider since goiters have multiple possible causes — some of which require treatment.
Treatment for goiter depends on how large your thyroid has grown, symptoms and what caused it.
No treatment/watchful waiting
If the goiter is small and isn’t bothering you, your healthcare provider may decide that it doesn’t need to be treated. However, they’ll carefully monitor your thyroid for any changes.
Medications
Medications for goiters may include one of the following:
- Increasing hormone production. An underactive thyroid is treated with a thyroid hormone replacement. The drug levothyroxine (Levoxyl, Thyquidity, others) replaces T-4 and results in the pituitary gland releasing less TSH. The drug liothyronine (Cytomel) may be prescribed as a T-3replacement. These treatments may decrease the size of the goiter.
- Reducing hormone production. An overactive thyroid may be treated with an anti-thyroid drug that disrupts hormone production. The most commonly used drug, methimazole (Tapazole), may also reduce the size of the goiter.
- Blocking hormone activities. Your health care provider may prescribe a drug called a beta blocker for managing symptoms of hyperthyroidism. These drugs — including atenolol (Tenormin), metoprolol (Lopressor) and others — can disrupt the excess thyroid hormones and lower symptoms.
- Managing pain. If inflammation of the thyroid results in pain, it’s usually treated with aspirin, naproxen sodium (Aleve), ibuprofen (Advil, Motrin IB, others) or related pain relievers. Severe pain may be treated with a steroid.
Surgery
You may need surgery to remove all or part of your thyroid gland (total or partial thyroidectomy) may be used to treat goiter with the following complications:
- Difficulty breathing or swallowing
- Thyroid nodules that cause hyperthyroidism
- Thyroid cancer
You may need to take thyroid hormone replacement, depending on the amount of thyroid removed.
Radioactive iodine treatment
Radioactive iodine is a treatment for an overactive thyroid gland. The dose of radioactive iodine is taken orally. The thyroid takes up the radioactive iodine, which destroys cells in the thyroid. The treatment lowers or eliminates hormone production and may decrease the size of the goiter.
As with surgery, you may need to take thyroid hormone replacement to maintain the appropriate levels of hormones.
Home/Self Care
Depending on your type of goiter, you may need to increase or decrease your iodine intake at home.
Your body gets iodine from your food. The recommended daily allowance is 150 micrograms. A teaspoon of iodized salt has about 250 micrograms of iodine. Too much iodine in the diet, however, can cause thyroid dysfunction.
Foods that contain iodine include:
- Saltwater fish and shellfish
- Seaweed
- Dairy products
- Soy products
Many goiters disappear with treatment, while others may increase in size. Speak with your doctor if your symptoms increase or become worse.
If your thyroid continues to make more hormones than you need, this can lead to hyperthyroidism. Not making enough hormones may lead to hypothyroidism.
Diagnosis and treatment of Chronic cough
- List of Common Diseases & Medical Disorders
- Buy Complete Premium Anatomy Notes (PDFs)
- Medmichihealthcare New posts
- Read All causes of disease short notes
- Read All diagnosis of disease short notes
- Read All treatment of disease short notes
- Subscribe Medmichihealthcare YouTube channel
Discover more from Medmichihealthcare
Subscribe to get the latest posts sent to your email.