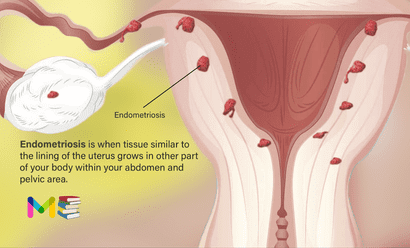
Endometriosis is when tissue similar to the lining of the uterus grows in other parts of your body within your abdomen and pelvic area. It often affects the ovaries, fallopian tubes and the tissue lining the pelvis. Rarely, endometriosis growths may be found beyond the area where pelvic organs are located. This can cause painful and heavy periods, as well as fertility issues.
The endometrium is the inner lining of your uterus. This tissue is what you shed during a menstrual period. Think of endometrium as layers of tissue that build up along the inside lining of your uterus. When you have a period, these layers fall away from the walls of your uterus and leave your body. If you get pregnant, the endometrium helps support the early phases of development.
Endometriosis is a condition that most commonly impacts people between the ages of 25 and 40. It can also happen to younger people during their teenage years. Although many people find relief from endometriosis symptoms after menopause, it can still cause discomfort and pain.
When you have endometriosis, endometrial-like tissue grows on other organs or structures. This tissue can grow within your abdomen, pelvis or even chest. This tissue is hormonally sensitive and can become inflamed during your menstrual cycle. These areas of endometrial-like tissue can cause ovarian cysts, superficial lesions, deeper nodules, adhesions (tissue that connects your organs and binds them together) and scar tissue within your body.
Table of Contents
Locations of endometriosis
A few places you can develop endometriosis include the:
- Outside and back of your uterus.
- Fallopian tubes.
- Ovaries.
- Vagina.
- Peritoneum (the lining of your abdomen and pelvis).
- Bladder and ureters.
- Intestines.
- Rectum.
- Diaphragm (a muscle near the bottom of your chest that plays an important role in breathing).
Symptoms of endometriosis
The main symptom of endometriosis is pelvic pain. It’s often linked with menstrual periods. Although many people have cramping during their periods, those with endometriosis often describe menstrual pain that’s far worse than usual. The pain also may become worse over time.
Common symptoms of endometriosis include:
- Painful periods. Pelvic pain and cramping may start before a menstrual period and last for days into it. You also may have lower back and stomach pain. Another name for painful periods is dysmenorrhea.
- Pain with sex. Pain during or after sex is common with endometriosis.
- Pain with bowel movements or urination. You’re most likely to have these symptoms before or during a menstrual period.
- Excessive bleeding. Sometimes, you may have heavy menstrual periods or bleeding between periods.
- Infertility. For some people, endometriosis is first found during tests for infertility treatment.
- Other symptoms. You may have fatigue, diarrhea, constipation, bloating or nausea. These symptoms are more common before or during menstrual periods.
The seriousness of your pain may not be a sign of the number or extent of endometriosis growths in your body. You could have a small amount of tissue with bad pain. Or you could have lots of endometriosis tissue with little or no pain.
Still, some people with endometriosis have no symptoms. Often, they find out they have the condition when they can’t get pregnant or after they get surgery for another reason.
For those with symptoms, endometriosis sometimes may seem like other conditions that can cause pelvic pain. These include pelvic inflammatory disease or ovarian cysts. Or it may be confused with irritable bowel syndrome (IBS), which causes bouts of diarrhea, constipation and stomach cramps. IBS also can happen along with endometriosis. This makes it harder for your health care team to find the exact cause of your symptoms.
You can also read the symptoms and causes of adenomyosis
Causes of endometriosis
The exact cause of endometriosis is not yet fully understood. When you have endometriosis, tissue similar to the lining of your uterus grows in the wrong places. When it develops in places like the outside of your uterus, fallopian tubes, ovaries, intestine and within your pelvic cavity, it can cause painful symptoms. This pain is related to increased inflammation and often fibrosis and adhesions.
Some of the possible causes of endometriosis include:
- Retrograde menstruation. This is when menstrual blood flows back through the fallopian tubes and into the pelvic cavity instead of out of the body. The blood contains endometrial cells from the inner lining of the uterus. These cells may stick to the pelvic walls and surfaces of pelvic organs. There, they might grow and continue to thicken and bleed over the course of each menstrual cycle.
- Transformed peritoneal cells. Experts suggest that hormones or immune factors might help transform cells that line the inner side of the abdomen, called peritoneal cells, into cells that are like those that line the inside of the uterus.
- Embryonic cell changes. Hormones such as estrogen may transform embryonic cells, cells in the earliest stages of development, into endometrial-like cell growths during puberty.
- Surgical scar complication.Endometrial cells may attach to scar tissue from a cut made during surgery to the stomach area, such as a C-section.
- Endometrial cell transport. The blood vessels or tissue fluid system may move endometrial cells to other parts of the body.
- Immune system condition. A problem with the immune system may make the body unable to recognize and destroy endometriosis tissue.
Stages of endometriosis
Endometriosis has four stages or types. Different factors determine the stage of the disorder. These factors can include the location, number, size, and depth of endometrial implants. Stages of endometriosis include:
- Stage 1 (Minimal): In minimal endometriosis, there are small lesions or wounds and shallow endometrial implants on your ovaries. There may also be inflammation in or around your pelvic cavity.
- Stage 2 (Mild): Mild endometriosis involves light lesions and shallow implants on the ovaries and the pelvic lining.
- Stage 3 (Moderate): Moderate endometriosis involves many deep implants on your ovaries and pelvic lining. There can also be more lesions.
- Stage 4 (Severe): The most severe stage of endometriosis involves many deep implants on your pelvic lining and ovaries. There may also be lesions on your fallopian tubes and bowels. There can also be cysts on one or both of your ovaries.
You can also read the causes and symptoms of ectopic pregnancy
Risk factors of endometriosis
Endometriosis usually develops years after the start of your menstrual cycle. It can be a painful condition. However, understanding its risk factors can help you determine whether you’re more likely to develop this condition and when you should talk with your doctor.
The following were some of the factors that can place you at a higher risk of developing endometriosis.
- Family history of endometriosis.
- The age you first start having periods. People who begin menstruating before age 11 may be at a higher risk.
- The length of your menstrual cycle (shorter time between periods) and the duration of flow (how many days of bleeding).
- Defects in your uterus or fallopian tubes.
- Never giving birth.
- Going through menopause at an older age.
- Having higher levels of estrogen in your body or a greater lifetime exposure to estrogen your body produces.
- Low body mass index.
Any health condition that prevents blood from flowing out of the body during menstrual periods also can be an endometriosis risk factor. So can conditions of the reproductive tract.
Complications of endometriosis
There are several medical complications that can happen if you have endometriosis. These include:
- Fertility issues: People with endometriosis may experience fertility issues (difficulty getting pregnant). This can sometimes be helped with treatment options like medications, surgery for endometriosis or fertility treatments like IVF.
- Bowel or bladder issues: People with endometriosis can also experience bowel or bladder issues. These may include pain with voiding or with bowel movements, or seeing blood in your urine (pee) or stool (poop). With severe endometriosis of your ureter (the tube that carries urine from your kidney to your bladder), you can occasionally get swelling of your kidney.
- Problems with the lungs or diaphragm: Endometriosis can occasionally impact your lung or diaphragm, which can lead to shortness of breath, chest pain or lung collapse during menstrual cycles.
- Chronic (long-term) pain: Chronic (long-term) pain is another issue related to endometriosis. Your healthcare provider will work with you to manage these issues to improve your daily life.
- Cancer: Endometriosis is associated with a small increased risk of developing epithelial ovarian cancer, mainly including clear cell and endometroid carcinomas. This risk is extremely low and no preventative screening is currently recommended.
You can also read the risk factors and complications of abnormal uterine bleeding
Prevention of endometriosis
Endometriosis isn’t a condition you can necessarily prevent. There are certain factors that can reduce your risk of developing the condition, but in some cases, you may still have endometriosis. There could be a genetic reason that some people develop endometriosis. If other people in your family (mother or grandmother) have been diagnosed with endometriosis, talk to your provider about your risk of also developing the condition.
A few factors that can reduce your risk of endometriosis include:
- Pregnancy.
- Breastfeeding.
- Maintaining a weight that’s healthy for you.
- Starting your menstrual period at a later age.
Diagnosis of endometriosis
The symptoms of endometriosis can be similar to the symptoms of other conditions, such as ovarian cysts and pelvic inflammatory disease. The condition also shares similar symptoms with irritable bowel syndrome (IBS), which can prolong diagnosis.
At the core of treating your pain is getting an accurate diagnosis. It’s important to note that the diagnosis process may vary. In some situations, it can take 4 to 11 years from the onset of symptoms to diagnosis, according to research published in 2019.
Your doctor will perform one or more of the following tests to diagnose endometriosis. These include:
- Detailed history: Your doctor will note your symptoms and personal or family history of endometriosis. A general health assessment may also be performed to determine if there are any other signs of a long-term disorder.
- Physical exam: During a pelvic exam, your doctor will use a speculum and light to see inside of the vagina and cervix. They will also manually feel your abdomen for cysts or scars behind the uterus.
- Ultrasound: Your doctor may use a transvaginal ultrasound or an abdominal ultrasound. In a transvaginal ultrasound, a probe is inserted into your vagina. Both types of ultrasound provide images of your reproductive organs. They can help your doctor identify cysts associated with endometriosis, but they aren’t effective in ruling out the disease.
- Laparoscopy: The only certain method for identifying endometriosis is by viewing it directly. This is done by a minor surgical procedure known as laparoscopy. Once diagnosed, the tissue can be removed in the same procedure.
- Magnetic resonance imaging (MRI): This exam uses a magnetic field and radio waves to make images of the organs and tissues within the body. For some, an MRI helps with surgical planning. It gives your surgeon detailed information about the location and size of endometriosis growths.
You can also read the prevention and diagnosis of polymorphic eruption of pregnancy
Treatment of endometriosis
Your healthcare provider will help create your treatment plan for endometriosis based on a few factors, including:
- The severity of your endometriosis.
- Your plans for future pregnancies.
- Your age.
- The severity of your symptoms (often pain).
In many cases, your treatment plan will focus primarily on managing your pain and improving fertility issues (if you are planning on a future pregnancy). This can be done through medications and surgery.
Medications are often used to help control the symptoms of endometriosis. These can include pain medications and hormone therapies.
Hormonal options
Hormonal options for suppressing endometriosis can include:
- Birth control: There are multiple forms of hormonal suppression options including combination options using estrogen and progesterone or progesterone-only options. These come in multiple forms including oral birth control pills, patch, vaginal ring, birth control shot, Nexplanon implant or IUD. This hormonal treatment often helps people have lighter, less painful periods. These are not options for patients attempting pregnancy.
- Gonadotropin-releasing hormone (GnRH) medications: This medication is actually used to stop the hormones that cause your menstrual cycle. This basically puts your reproductive system on hold as a way to relieve your pain. GnRH medications can be taken as an oral pill (by mouth), a shot or a nasal spray.
- Danazol (Danocrine): This is another form of hormonal medication that stops the production of the hormones that cause you to have a period. While taking this medication for endometriosis symptoms, you may have the occasional menstrual period, or they might stop entirely.
With all of these medications, it’s important to note that your symptoms can come back if you stop taking the medication. These medications aren’t recommended during pregnancy or if you are actively attempting to achieve pregnancy. Talk to your healthcare provider about the pros and cons of each medication before starting.
Medications
Medications for endometriosis pain relief can include:
- Over-the-counter pain relief.
- Non-steroidal anti-inflammatory drugs (NSAIDs).
In some cases, your provider might recommend surgery as a way to confirm and treat endometriosis. There are always risks to a surgical procedure. However, surgery for endometriosis can be an effective way to relieve pain and, in some cases, improve your fertility.
Endometriosis is considered a chronic disease. Many people experience relief from endometriosis pain after surgery, but the symptoms may return within a few years. The severity of your endometriosis could play a part in how quickly, if at all, it comes back after surgery. Your provider might suggest combining a surgical procedure with medications for the best outcome. Your provider may recommend pelvic floor physical therapy with or without medications for central nerve pain.
Surgical options
Surgical options to treat endometriosis include:
- Laparoscopy: In this procedure, your surgeon will make a very small cut in your abdomen (< 1 centimeter) and insert a thin tube-like tool called a laparoscope into your body. This tool can be used to see inside your body and identify endometriosis with a high-definition camera. Additional 5-millimeter instruments can then be used to excise and remove lesions.
- Hysterectomy: In severe cases, your surgeon may suggest removing your uterus based on the amount of endometriosis and scar tissue present, if you have other uterine conditions like adenomyosis and your desire for future fertility. If you have a hysterectomy, areas of endometriosis should still be excised to optimize your pain relief.
If you have endometriosis and are trying to achieve pregnancy, in vitro fertilization (IVF) may help you achieve this goal.
In some cases, endometriosis can go away on its own. Over time, endometriosis lesions can occasionally get smaller, and you may have fewer of them. This can also happen after menopause, which is often related to a drop in the amount of estrogen in your body.
For many people, endometriosis needs to be continuously treated to control symptoms like pain. It’s important to maintain a regular appointment schedule with your healthcare provider so that you can work together on managing your condition long term.
Over time, the endometrial-like tissue that grows outside of your uterus can cause cysts, adhesions and scar tissue. This can cause you to experience long-term (chronic) pain, especially during menstrual periods. Many people with endometriosis may also have difficulties getting pregnant. Treatment can sometimes help with this issue.
As you age and go through menopause, the symptoms of menopause may improve. This is related to the hormonal changes your body goes through during menopause.
- List of Common Diseases & Medical Disorders
- Buy Complete Premium Anatomy Notes (PDFs)
- Medmichihealthcare New posts
- Read All causes of disease short notes
- Read All diagnosis of disease short notes
- Read All treatment of disease short notes
- Subscribe Medmichihealthcare YouTube channel
Discover more from Medmichihealthcare
Subscribe to get the latest posts sent to your email.