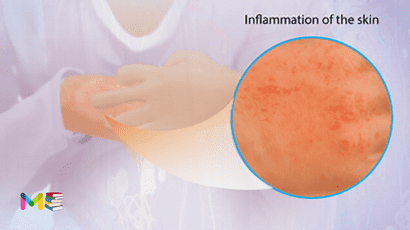
Eczema (atopic dermatitis) is a condition that causes dry, itchy and inflamed skin. Eczema is a type of dermatitis, which is long lasting (chronic) and tends to flare sometimes. It can be irritating but it’s not contagious. It typically starts during infancy or early childhood age and can persist into adulthood. However, it can occur in people of any age.
Atopic dermatitis is common and affects over 31 million Americans. Infants are prone to eczema, and 10% to 20% will have it. However, nearly half of all infants diagnosed with eczema outgrow the condition or have significant improvement as they develop older.
Table of Contents
Symptoms of eczema
Atopic dermatitis symptoms can appear anywhere on the body and can vary largely from person to person. Symptoms of eczema include:
- Itchiness (pruritus)
- Rash on swollen skin that varies in color depending on your skin color
- Dry, cracked skin
- Small, raised bumps, on brown or Black skin
- Oozing and crusting
- Darkening of the skin around the eyes
- Raw, sensitive skin from scratching
- Thickened skin
It often begins before age 5 and may continue into the teen and adult age. For some people, it flares and then clears up for a time, even for many years.
Symptoms can show up anywhere on your skin. Common places include, Hands, Neck, Elbows, Ankles, Knees, Feet, Face, especially cheeks, In and around ears and also on the Lips. Other less common places include, Nipples, Breasts, Folds of skin near your vagina (vulva) and the Penis.
When to seek medical attention
You should seek a medical attention if:
- Has symptoms of atopic dermatitis
- You are so uncomfortable that the condition is affecting sleep and daily activities
- Has symptoms even after trying self-care steps
- Has a skin infection, like new streaks, pus, yellow scabs
- You or your child has a fever and rash that looks infected.
Triggers of eczema
An eczema flare-up happens when one or more of it symptoms appear on the skin. Common triggers of atopic dermatitis include:
- sweating
- chemicals or preservatives found in cleansers and detergents
- scented products
- cigarette smoke
- external allergens such as pollens, mold, dust, or dust mites
- rough scratchy material, like wool
- synthetic fabrics
- temperature changes
- stress
- food allergies
- upper respiratory infections
- animal dander
You can also read the symptoms and triggers of asthma
Types of eczema
There are many types of atopic dermatitis, and each type has their unique triggers that can affect your skin’s barrier function. These include:
- Atopic dermatitis.
- Dyshidrotic eczema.
- Contact dermatitis.
- Neurodermatitis.
- Seborrheic dermatitis.
- Nummular eczema.
In some cases, it is possible to have more than one type at same time.
Causes of eczema
The first signs of atopic dermatitis are itchiness, dry skin and a rash. These signs indicate that you came into contact with a trigger in your environment that caused your symptoms to start or flare up. Several factors cause it, including:
- Gene. You’re more likely to have eczema if there’s a history of eczema or dermatitis in your family.
- Overreactive Immune system: If you have eczema, your immune system overreacts to small irritants or allergens (triggers) in your environment.
- Environmental factor. There’s a lot in your environment that can irritate your skin. Some examples include exposure to smoke, air pollutants, harsh soaps, fabrics such as wool, and some skin care products
- Emotional triggers: Your mental health could affect the health of your skin, which can cause a flare-up of eczema symptoms. For example, having high levels of stress, anxiety or depression.
A weak skin barrier function may also trigger an immune system response that can cause inflamed skin and other symptoms.
Atopic dermatitis can look different on each person diagnosed with the condition. If you have a dark skin tone, the rash can be purple, brown or gray. If you have a light skin tone, the rash can look pink, red or purple.
You can also read the types and causes of pneumonia
Risk factors of eczema
There are very few factors that can increase your risk of getting eczema. These include:
- Children who suffer from dermatitis, asthma, allergies or hay fever as well as adults who develop these conditions before age 30.
- People with family members who have eczema are also at higher risk of developing the condition.
Complications of eczema
The complications of atopic dermatitis include:
- Chronic itchy and scaly skin. A skin condition called neurodermatitis (lichen simplex chronicus) starts with a patch of itchy skin. You scratch the area, which provides only temporary relief. Scratching actually makes the skin itchier because it activates the nerve fibers in your skin. Over time, you may scratch out of habit. This condition can cause the affected skin to become discolored, thick and leathery.
- Patches of skin. Patches that’s darker or lighter than the surrounding area. This complication after the rash has healed is called post-inflammatory hyperpigmentation or hypopigmentation. It’s more common in people with brown or Black skin. It might take several months for the discoloration to fade.
- Food allergies. People with atopic dermatitis often develop food allergies. One of the main symptoms of this condition is hives (urticaria).
- Skin infections. Repeated scratching that breaks the skin can cause open sores and cracks. These increase the risk of infection from bacteria and viruses. These skin infections can spread and become life-threatening.
- Irritant hand dermatitis. This especially affects people whose hands are often wet and exposed to harsh soaps, detergents and disinfectant at work.
- Allergic contact dermatitis. This condition is common in people with atopic dermatitis. Allergic contact dermatitis is an itchy rash caused by touching substances you’re allergic to. The color of the rash varies depending on your skin color.
- Asthma and hay fever. Many people with atopic dermatitis develop asthma and hay fever. This can happen before or after developing atopic dermatitis.
- Mental health conditions. Atopic dermatitis is associated with depression and anxiety. This may be related to the constant itching and sleep problems common among people with atopic dermatitis.
- Sleep problems. The itchiness of atopic dermatitis can interfere with sleep.
You can also read the risk factors and complications of stomach flu
Prevention of eczema
There are several steps you can take in preventing eczema flare-ups and outbreaks. These steps include:
- Avoid irritants and allergens.
- Take baths or showers with warm, not hot, water.
- Moisturize your skin regularly or when your skin becomes dry. Seal in moisture after a bath or shower by immediately applying moisturizer to your skin.
- Stay hydrated and drink at least eight glasses of water each day. Water helps keep your skin moist.
- Wear loose clothes made of cotton and other natural materials. Wash new clothing before wearing it. Avoid wool or synthetic fibers.
- Use a humidifier if dry air makes your skin dry.
- Manage your stress and emotional triggers. See a psychiatrist for medication and a therapist for counseling if you’re experiencing symptoms of poor mental/emotional health.
Diagnosis of eczema
Your doctor will diagnose atopic dermatitis after a physical examination, where they can take a close look at your skin. Most often, people receive an eczema diagnosis as a child, as it’s common among children, but a diagnosis can happen at any age when symptoms arise or when having flare-up.
During your examination, your doctor may ask the following questions to easily learn more about your symptoms. These include:
- Did you use any products to try to treat your skin?
- Where do you have symptoms on your body?
- Do you have any medical conditions like allergies or asthma?
- Do you have a history of eczema in your family?
- How long have you had symptoms?
- Do you take hot showers?
- Have you noticed something triggers or worsens your symptoms like certain soaps or detergents?
- Do your symptoms affect your ability to sleep or perform your daily activities?
- Is there anything that makes your symptoms worse?
The symptoms of atopic dermatitis can look similar to other related conditions. Your doctor may offer tests to rule out other conditions and spot your actual diagnosis. These tests include:
- Allergy test. A patch test can pinpoint certain allergens that trigger symptoms, like skin allergies associated with contact dermatitis
- Blood tests. To check for causes of the rash that might be unrelated to dermatitis.
- Skin biopsy. To distinguish one type of dermatitis from another.
You can also read the Prevention and diagnosis of chronic cough
Treatment of eczema
Management of atopic dermatitis (eczema) start with regular moisturizing and other self-care habits. If these don’t help, your doctor might suggest medicated creams or lotions that control itching and help repair skin rashes. These are sometimes combined with other forms of treatments.
Atopic dermatitis can be persistent, and you may need to try different treatments methods over months or years to control it. And even when treatment is successful, symptoms may still return as flare.
Medications used for atopic dermatitis:
- Medicated products applied to the skin. Many options are available to help control itching and repair the skin. Products are available in various strengths and as creams, gels and ointments. Talk with your health care provider about the options and your preferences. Whatever you use, apply it as directed (often twice a day), before you moisturize. Overuse of a corticosteroid product applied to the skin may cause side effects, such as thinning skin.Creams or ointments with a calcineurin inhibitor might be a good option for those over age 2. Examples include tacrolimus (Protopic) and pimecrolimus (Elidel). Apply it as directed, before you moisturize. Avoid strong sunlight when using these products.The Food and Drug Administration requires that these products have a black box warning about the risk of lymphoma. This warning is based on rare cases of lymphoma among people using topical calcineurin inhibitors. After 10 years of study, no causal relationship between these products and lymphoma and no increased risk of cancer have been found.
- Pills that control inflammation. For more-severe eczema, your health care provider may prescribe pills to help control your symptoms. Options might include cyclosporine, methotrexate, prednisone, mycophenolate and azathioprine. These pills are effective but can’t be used long term because of potential serious side effects.
- Drugs to fight infection. Your health care provider may prescribe antibiotic pills to treat an infection.
- Other options for severe eczema. The injectable biologics (monoclonal antibodies) dupilumab (Dupixent) and tralokinumab (Adbry) might be options for people with moderate to severe disease who don’t respond well to other treatment. Studies show that it’s safe and effective in easing the symptoms of atopic dermatitis. Dupilumab is for people over age 6. Tralokinumab is for adults.
Medical therapies used for atopic dermatitis:
- Phototherapy. This treatment is used for people who either don’t get better with topical treatments or rapidly flare again after treatment. The simplest form of light therapy (phototherapy) involves exposing the affected area to controlled amounts of natural sunlight. Other forms use artificial ultraviolet A (UVA) and narrow band ultraviolet B (UVB) alone or with drugs. Though effective, long-term light therapy has harmful effects, including premature skin aging, changes in skin color (hyperpigmentation) and an increased risk of skin cancer. For these reasons, phototherapy is less commonly used in young children and is not given to infants. Talk with your health care provider about the pros and cons of light therapy.
- Wet dressings. An effective, intensive treatment for severe eczema involves applying a corticosteroid ointment and sealing in the medication with a wrap of wet gauze topped with a layer of dry gauze. Sometimes this is done in a hospital for people with widespread lesions because it’s labor intensive and requires nursing expertise. Or ask your health care provider about learning how to use this technique at home safely.
- Relaxation, behavior modification and biofeedback. These approaches may help people who scratch out of habit.
- Counseling. If you’re embarrassed or frustrated by your skin condition, it can help to talk with a therapist or other counselor.
Treatment of eczema in babies:
- Avoiding extreme temperatures
- Identifying and avoiding skin irritants
- Giving your baby a short bath in warm water and applying a cream or ointment while the skin is still damp
You should see your baby’s doctor, if these steps don’t improve the rash or it looks infected. Your baby might need a prescription medication to control the rash or treat an infection. Your doctor might also recommend an oral antihistamine to help lessen the itchiness and cause drowsiness, which may be helpful for nighttime itching and also discomfort. Before any self-care or home remedies to treat atopic dermatitis, make sure to seek the advice of your healthcare provider first.
- List of Common Diseases & Medical Disorders
- Buy Complete Premium Anatomy Notes (PDFs)
- Medmichihealthcare New posts
- Read All causes of disease short notes
- Read All diagnosis of disease short notes
- Read All treatment of disease short notes
- Subscribe Medmichihealthcare YouTube channel
Discover more from Medmichihealthcare
Subscribe to get the latest posts sent to your email.