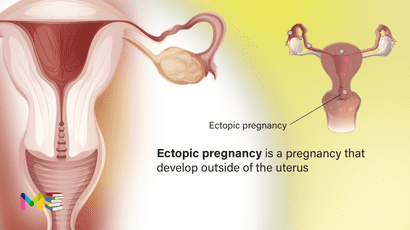
Ectopic pregnancy is a condition whereby a pregnancy develop outside of the uterus. This occurs when a fertilized egg implants in a location that can’t support its growth.
An ectopic pregnancy often happens in your fallopian tube (a structure that connects your ovaries and uterus).
Ectopic pregnancies more rarely can occur in your ovary, abdominal cavity or cervix. Pregnancies can’t continue if they’re ectopic because only your uterus is meant to carry a pregnancy. The fertilized egg can’t survive, and the growing tissue may cause life-threatening bleeding, if left untreated.
In a healthy pregnancy, the fertilized egg attaches itself to the lining of the uterus. In an ectopic pregnancy, the egg attaches itself somewhere outside the uterus usually to the inside of a fallopian tube.
Ectopic pregnancies occur in about 2% of all pregnancies.
Table of Contents
Symptoms of ectopic pregnancy
Nausea and breast soreness are common symptoms in both ectopic and uterine pregnancies. The following symptoms are more common in an ectopic pregnancy and can indicate a medical emergency:
- severe pain that occurs on one side of the abdomen
- sharp waves of pain in the abdomen, pelvis, shoulder, or neck
- light to heavy vaginal spotting or bleeding
- rectal pressure
- dizziness or fainting
You should contact your doctor or seek immediate treatment if you know that you’re pregnant and have any of these symptoms.
You can also read about symptoms and causes of preeclampsia.
Causes of ectopic pregnancy
In most cases, conditions that slow down or block the movement of the egg down your fallopian tube cause ectopic pregnancy. This could happen because:
- You have scar tissue, adhesions or inflammation from a prior pelvic surgery.
- Your fallopian tubes have damage, such as from a sexually transmitted infection (STI).
- You were born with an irregularly-shaped fallopian tube.
- You have a growth blocking your fallopian tube.
Your doctor will give you more specific information about ectopic pregnancy.
Risk factors of ectopic pregnancy
Some things that make you more likely to have an ectopic pregnancy are:
- Inflammation or infection. Sexually transmitted infections, such as gonorrhea or chlamydia, can cause inflammation in the tubes and other nearby organs, and increase your risk of an ectopic pregnancy.
- Previous ectopic pregnancy. If you’ve had this type of pregnancy before, you’re more likely to have another.
- Fertility treatments. Some research suggests that women who have in vitro fertilization (IVF) or similar treatments are more likely to have an ectopic pregnancy. Infertility itself may also raise your risk.
- Tubal surgery. Surgery to correct a closed or damaged fallopian tube can increase the risk of an ectopic pregnancy.
- Smoking. Cigarette smoking just before you get pregnant can increase the risk of an ectopic pregnancy. The more you smoke, the greater the risk.
- Choice of birth control. The chance of getting pregnant while using an intrauterine device (IUD) is rare. However, if you do get pregnant with an intrauterine device (IUD) in place, it’s more likely to be ectopic. Tubal ligation, a permanent method of birth control commonly known as “having your tubes tied,” also raises your risk, if you become pregnant after this procedure.
Complication of ectopic pregnancy
- An ectopic pregnancy is a medical emergency. Your uterus is the only organ that can hold a growing fetus. It can stretch and expand as the fetus grows. Your fallopian tubes aren’t as flexible. They can burst as the fertilized egg develops. If this happens, it can cause severe, life-threatening internal bleeding. This is dangerous.
- An ectopic pregnancy needs to be treated right away to avoid injury to your fallopian tube and other organs, internal bleeding and possibly, death.
Prevention of ectopic pregnancy
Prediction and prevention aren’t possible in every case. You may be able to reduce your risk through good reproductive health maintenance. Have your partner wear a condom during sex and limit your number of sexual partners. This reduces your risk for STDs, which can cause PID, a condition that can cause inflammation in the fallopian tubes.
Maintain regular visits with your doctor, including regular gynecological exams and regular STD screenings. Taking steps to improve your personal health, such as quitting smoking, is also a good preventive strategy.
You can also read about risk factors and prevention of diabetes.
Diagnosis of ectopic pregnancy
Most people don’t know that their pregnancy is ectopic until they visit their pregnancy care provider for a prenatal appointment, bloodwork or ultrasound. Your provider may suspect an ectopic pregnancy based on what happens at this appointment.
To diagnose an ectopic pregnancy, your provider will perform several tests. These tests include:
- A pelvic exam: can help your doctor identify areas of pain, tenderness, or a mass in the fallopian tube or ovary. However, your doctor can’t diagnose an ectopic pregnancy by examining you. You’ll need blood tests and an ultrasound.
- A blood test: You provider may test your blood to see how much of the hormone human chorionic gonadotropin (HCG) you have in your body. Your body only makes HCG during pregnancy. A low amount may indicate an ectopic pregnancy because HCG levels increase dramatically when a fertilized egg implants in your uterus.
- An ultrasound exam: An ultrasound uses sound waves to create a picture of your body’s internal structures. Your provider will use this test to see where the fertilized egg has implanted.
- A urine test: This test involves either peeing on a test strip or into a cup in your provider’s office and then having a test strip dipped into the urine sample.
- Culdocentesis: can also be performed If your provider suspects the ectopic pregnancy has ruptured, but that is rarely used.
Once your provider has confirmed an ectopic pregnancy and determined where the fertilized egg has implanted, they’ll discuss a treatment plan with you. An ectopic pregnancy is an emergency and treatment is very important.
Treatment of ectopic pregnancy
A fertilized egg can’t develop normally outside the uterus. To prevent life-threatening complications, the ectopic tissue needs to be removed. Depending on your symptoms and when the ectopic pregnancy is discovered, this may be done using medication, laparoscopic surgery or abdominal surgery.
Medication management
An early ectopic pregnancy without unstable bleeding is most often treated with a medication called methotrexate, which stops cell growth and dissolves existing cells. The medication is given by injection. It’s very important that the diagnosis of ectopic pregnancy is certain before receiving this treatment.
After the injection, your doctor will order another human chorionic gonadotropin (HCG) test to determine how well treatment is working, and if you need more medication.
In some cases, your provider may suggest using a medication called methotrexate to stop the fertilized egg from growing, ending the pregnancy. The medication shouldn’t damage your fallopian tubes. You can’t use this medication if your fallopian tube has already ruptured.
Medical procedures
Salpingostomy and salpingectomy are two laparoscopic surgeries used to treat some ectopic pregnancies. In these procedure, a small incision is made in the abdomen, near or in the navel. Next, your doctor uses a thin tube equipped with a camera lens and light (laparoscope) to view the tubal area.
In a salpingostomy, the ectopic pregnancy is removed and the tube left to heal on its own. In a salpingectomy, the ectopic pregnancy and the tube are both removed.
Which procedure you have depends on the amount of bleeding and damage and whether the tube has ruptured. Also a factor is whether your other fallopian tube is normal or shows signs of prior damage.
If the ectopic pregnancy is causing heavy bleeding, you might need emergency surgery. This can be done laparoscopically or through an abdominal incision (laparotomy). In some cases, the fallopian tube can be saved. Typically, however, a ruptured tube must be removed.
Coping and support after ectopic pregnancy
The long-term outlook after an ectopic pregnancy depends on whether it caused any physical damage. Most people who have ectopic pregnancies go on to have healthy pregnancies. If both fallopian tubes are still intact, or even just one, the egg can be fertilized as normal. However, if you have a preexisting reproductive problem, that can affect your future fertility and increase your risk of future ectopic pregnancy. This is especially the case if the preexisting reproductive problem has previously led to an ectopic pregnancy.
Surgery may scar the fallopian tubes, and it can make future ectopic pregnancies more likely. If the removal of one or both fallopian tubes is necessary, speak to your doctor about possible fertility treatments. An example is in vitro fertilization that involves implanting a fertilized egg into the uterus.
Pregnancy loss, no matter how early, can be devastating. You can ask your doctor if there are available support groups in the area to provide further support after loss. Take care of yourself after this loss through rest, eating healthy foods, and exercising when possible. Give yourself time to grieve.
Remember that many women go on to have healthy pregnancies and babies. When you’re ready, talk to your doctor about ways you can ensure that your future pregnancy is a healthy one.
Subscribe YouTube Channel
- Subscribe Medmichihealthcare YouTube channel
- List of Common Diseases & Medical Disorders
- Buy Complete Premium Anatomy Notes (PDFs)
- Medmichihealthcare New posts
- Read All causes of disease short notes
- Read All diagnosis of disease short notes
- Read All treatment of disease short notes
Discover more from Medmichihealthcare
Subscribe to get the latest posts sent to your email.