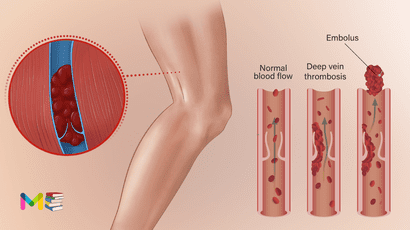
Deep vein thrombosis (also known as venous thrombosis) occurs when a blood clot (thrombus) develops in veins deep in your body because your veins are injured or the blood flowing through them is too sluggish.
The blood clots may partially or completely block blood flow through your vein. Most DVTs happen in your lower leg, thigh or pelvis, but they also can occur in other parts of your body including your arm, brain, intestines, liver or kidney.
Deep vein thrombosis can be serious because blood clots in the veins can break loose. The clots can then travel through the bloodstream and get stuck in the lungs, blocking blood flow (pulmonary embolism). When DVT and pulmonary embolism occur together, it’s called venous thromboembolism (VTE).
Table of Contents
Symptoms of deep vein thrombosis
Common DVT symptoms include:
- swelling in your foot, ankle, or leg, usually on one side
- cramping pain in your affected leg that usually begins in your calf
- severe, unexplained pain in your foot and ankle
- an area of skin that feels warmer than the skin in the surrounding areas
- the skin over the affected area turning pale or reddish, or bluish color, depending on skin tone
People with an upper extremity DVT, or a blood clot in the arm, may not experience symptoms. If they do, common symptoms include:
- neck pain
- shoulder pain
- swelling in the arm or hand
- blue- or darker-tinted skin color
- pain that moves from the arm to the forearm
- weakness in the hand
People may not find out they have DVT until they’ve undergone emergency treatment for a pulmonary embolism (blood clot in the lung).
A pulmonary embolism can happen when a DVT clot has moved from the arm or leg into the lung. When an artery in the lung becomes blocked, it’s life threatening and requires emergency care.
Causes of deep vein thrombosis
These conditions can increase your risk of a deep vein thrombosis:
- Having an inherited (genetic) condition increases your risk of blood clots.
- Having cancer and some of its treatments (chemotherapy).
- Having a history of deep vein thrombosis in yourself or your family.
- Having limited blood flow in a deep vein because of an injury, surgery or immobilization.
- Not moving for long periods of time, like sitting for a long time on trips in a car, truck, bus, train or airplane or being immobile after surgery or a serious injury.
- Being pregnant or having recently delivered a baby.
- Being older than 40 (although a DVT can affect people of any age).
- Having overweight/obesity.
- Having an autoimmune disease, like lupus, vasculitis or inflammatory bowel disease.
- Using tobacco products.
- Having varicose veins.
- Taking birth control pills or hormone therapy.
- Having a central venous catheter or pacemaker.
- Having COVID-19.
You can also read about causes and symptoms of stroke
Risk factors of developing deep vein thrombosis
Many things can increase the risk of developing deep vein thrombosis (DVT). The more risk factors you have, the greater your risk of DVT. Risk factors for DVT include:
- Lack of movement. When the legs don’t move for a long time, the calf muscles don’t squeeze (contract). Muscle contractions help blood flow. Sitting for a long time, such as when driving or flying, increases the risk of DVT. So does long-term bed rest, which may result from a lengthy hospital stay or a medical condition such as paralysis.
- Age. Being older than 60 increases the risk of DVT. But DVT can occur at any age.
- Injury or surgery. Injury to the veins or surgery can increase the risk of blood clots.
- Pregnancy. Pregnancy increases the pressure in the veins in the pelvis and legs. The risk of blood clots from pregnancy can continue for up to six weeks after a baby is born. People with an inherited clotting disorder are especially at risk.
- Birth control pills (oral contraceptives) or hormone replacement therapy.Both can increase the blood’s ability to clot.
- Being overweight or obese. Being overweight increases the pressure in the veins in the pelvis and legs.
- Smoking. Smoking affects how blood flows and clots, which can increase the risk of DVT.
- Cancer. Some cancers increase substances in the blood that cause the blood to clot. Some types of cancer treatment also increase the risk of blood clots.
- Heart failure. Heart failure increases the risk of DVT and pulmonary embolism. Because the heart and lungs don’t work well in people with heart failure, the symptoms caused by even a small pulmonary embolism are more noticeable.
- Inflammatory bowel disease. Crohn’s disease or ulcerative colitis increase the risk of DVT.
- Genetics. Some people have DNA changes that cause the blood to clot more easily. One example is factor V Leiden. This inherited disorder changes one of the clotting factors in the blood. An inherited disorder on its own might not cause blood clots unless combined with other risk factors.
- A personal or family history of DVT or pulmonary embolism (PE). If you or someone in your family has had one or both of these conditions, you might be at greater risk of developing DVT.
Sometimes, a blood clot in a vein can occur with no identifiable risk factor. This is called an unprovoked venous thromboembolism (VTE).
Complication of deep vein thrombosis
A major complication of DVT is a pulmonary embolism. You can develop a pulmonary embolism if a blood clot moves to your lungs and blocks a blood vessel.
This can cause serious damage to your lungs and other parts of your body. Get immediate medical help if you have signs of a pulmonary embolism. These signs include:
- dizziness
- sweating
- chest pain that gets worse with coughing or inhaling deeply
- rapid breathing
- coughing up blood
- rapid heart rate
You can also read about risk factors and complications of diabetes
Prevention of deep vein thrombosis
After you have a DVT, you’ll need to reduce your risk of future DVT/PE clots by:
- Taking your medications exactly as your healthcare provider tells you to.
- Keeping your follow-up appointments with your doctor and the laboratory. These tell your provider how well your treatment is working.
- Making lifestyle changes, such as eating healthier foods, being more active and avoiding tobacco products.
If you’ve never had a DVT, but have an increased risk of developing one, be sure to:
- Exercise your calf muscles if you need to sit still for a long time. Stand up and walk at least every half hour if you’re on a long flight. Or get out of the car every hour if you’re on a long road trip.
- Get out of bed and move around as soon as you can after you’re sick or have surgery. The sooner you move around, the less chance you have of developing a DVT.
- Take medications or use compression stockings after surgery (if your provider prescribes them) to reduce your risk of a clot.
- Follow up with your provider as directed and follow their recommendations to reduce your risk of a clot.
Diagnosis of deep vein thrombosis
Your healthcare provider will do a physical exam and review your medical history. You’ll also need to have imaging tests.
Tests to diagnose a deep vein thrombosis
- Venography. In this invasive test, your provider numbs the skin of your neck or groin and uses a catheter to inject a special dye (contrast material) into your veins to see if any blood clots are partially or completely blocking blood flow inside your veins. Venography is rarely used nowadays, but sometimes it is necessary
- Duplex venous ultrasound. This is the most common test for diagnosing a DVT because it is non-invasive and widely available. This test uses ultrasound waves to show blood flow and blood clots in your veins. A vascular ultrasound technologist applies pressure while scanning your arm or leg. If the pressure doesn’t make your vein compress, it could mean there’s a blood clot. If the results of the duplex ultrasound aren’t clear, your provider can use another imaging test
- Computed tomography (CT) scan is a type of X-ray that shows structures inside your body. Your provider may use a CT scan to find a DVT in your abdomen, pelvis or brain, as well as blood clots in your lung (pulmonary embolism).
- Magnetic Resonance Imaging (MRI) or Magnetic Resonance Venography (MRV). MRI shows pictures of organs and structures inside your body. MRV shows pictures of the veins in specific locations in your body. In many cases, MRI and MRV can offer more information than a duplex ultrasound or CT scan.
If your doctor thinks you may have a genetic or acquired clotting disorder, you may need to have special blood tests. This may be important if:
- You have a history of blood clots that your provider can’t link to any other cause.
- You have a blood clot in an unusual location, such as in a vein from your intestines, liver, kidney or brain.
- You have a strong family history of blood clots.
- You have a family history of a specific genetic clotting disorder.
You can also read about Prevention and diagnosis of high blood pressure
Treatment of deep vein thrombosis
There are three main goals to DVT treatment.
- Prevent the clot from getting bigger.
- Prevent the clot from breaking loose and traveling to the lungs.
- Reduce the chances of another DVT.
Treatment options of deep vein thrombosis include:
- Blood thinners. These medicines, also called anticoagulants, help prevent blood clots from getting bigger. Blood thinners reduce the risk of developing more clots.Blood thinners may be taken by mouth or given by intravenous (IV) or an injection under the skin. There are many different types of blood-thinning drugs used to treat DVT. Together, you and your health care provider will discuss their benefits and risks to determine the best one for you.You might need to take blood thinner pills for three months or longer. It’s important to take them exactly as prescribed to prevent serious side effects.People who take a blood thinner called warfarin (Jantoven) need regular blood tests to monitor levels of the drug in the body. Certain blood-thinning medications are not safe to take during pregnancy.
- Clot busters (thrombolytics). These drugs are used for more-serious types of DVT or PE, or if other medications aren’t working.Clot busters are given by or through a tube (catheter) placed directly into the clot. They can cause serious bleeding, so they’re usually only used for people with severe blood clots.
- Filters. If you can’t take medicines to thin your blood, a filter may be placed into a large vein — the vena cava — in your belly (abdomen). A vena cava filter prevents clots that break loose from lodging in the lungs.
- Support stockings (compression stockings). These special knee socks help prevent blood from pooling in the legs. They help reduce leg swelling. Wear them on your legs from your feet to about the level of your knees. For DVT, you typically wear these stockings during the day for a few years, if possible.
Subscribe YouTube Channel
- Subscribe Medmichihealthcare YouTube channel
- List of Common Diseases & Medical Disorders
- Buy Complete Premium Anatomy Notes (PDFs)
- Medmichihealthcare New posts
- Read All causes of disease short notes
- Read All diagnosis of disease short notes
- Read All treatment of disease short notes
Discover more from Medmichihealthcare
Subscribe to get the latest posts sent to your email.
Sir can you provide the PPT regarding this chapter