Chronic obstructive pulmonary disease (COPD) is a chronic inflammatory lung disease that causes obstructed airflow from the lungs. It is a group of diseases that includes chronic bronchitis and emphysema. Over time, COPD makes it harder to breathe. You can’t reverse lung damage, but lifestyle changes and medication changes can help you manage the symptoms.
Emphysema and chronic bronchitis are the two most common conditions that contribute to COPD. These two conditions usually occur together and can vary in severity among individuals with COPD.
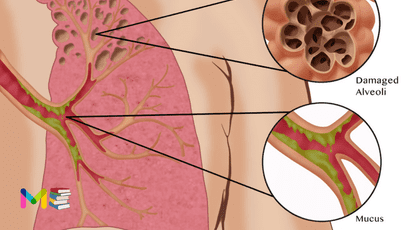
Chronic bronchitis is inflammation of the lining of the bronchial tubes, which carry air to and from the air sacs (alveoli) of the lungs. It’s characterized by daily cough and mucus (sputum) production.
Emphysema is a condition in which the alveoli at the end of the smallest air passages (bronchioles) of the lungs are destroyed as a result of damaging exposure to cigarette smoke and other irritating gases and particulate matter.
Although COPD is a progressive disease that gets worse over time, COPD is treatable. With proper management, most people with COPD can achieve good symptom control and quality of life, as well as reduced risk of other associated conditions.
Table of Contents
Symptoms of chronic obstructive pulmonary disease
At first, symptoms of COPD can be quite mild. You might mistake them for a cold. Early symptoms include:
- occasional shortness of breath, especially after exercise
- mild but recurrent cough
- needing to clear your throat often, especially first thing in the morning
You might start making subtle changes, such as avoiding stairs and skipping physical activities.
Symptoms can get progressively worse and harder to ignore. As the lungs become more damaged, you may experience:
- shortness of breath, after even mild forms of exercise like walking up a flight of stairs
- wheezing, which is a type of higher-pitched noisy breathing, especially during exhalations
- chest tightness
- chronic cough, with or without mucus
- need to clear mucus from your lungs every day
- frequent colds, flu, or other respiratory infections
- lack of energy
In later stages of COPD, symptoms may also include:
- fatigue
- swelling of the feet, ankles, or legs
- weight loss
Symptoms are likely to be much worse if you currently smoke or are regularly exposed to secondhand smoke.
You can also read about symptoms and causes of lung cancer
Causes of chronic obstructive pulmonary disease
Smoking tobacco causes up to 90% of COPD cases. In the vast majority of people with COPD, the lung damage that leads to COPD is caused by long-term cigarette smoking. But there are likely other factors at play in the development of COPD. Other causes include:
- Alpha-1 antitrypsin (AAT) deficiency, a genetic disorder.
- Secondhand smoke.
- Air pollution.
- Workplace dust and fumes.
Smoking. Tobacco smoke irritates airways, triggering inflammation (irritation and swelling) that narrows the airways. Smoke also damages cilia so they can’t do their job of removing mucus and trapped particles from the airways.
Alpha-1-antitrypsin deficiency. In about 1% of people with COPD, the disease results from a genetic disorder that causes low levels of a protein called alpha-1-antitrypsin (AAt). AAt is made in the liver and secreted into the bloodstream to help protect the lungs. Alpha-1-antitrypsin deficiency can cause liver disease, lung disease or both.
Stages of chronic obstructive pulmonary disease
One measure of COPD is achieved by spirometry grading.
There are different grading systems, and one grading system is part of the GOLD classification. The GOLD classification is used for determining COPD severity and helping to form a prognosis and treatment plan.
There are four GOLD grades based on spirometry testing:
- grade 1: mild
- grade 2: moderate
- grade 3: severe
- grade 4: very severe
This is based on the spirometry test result of your FEV1. This is the amount of air you can breathe out of the lungs in the first second of a forced expiration. The severity increases as your FEV1 decreases.
The GOLD classification also takes into account your individual symptoms and history of acute exacerbations. Based on this information, your doctor can assign a letter group to you to help define your COPD grade.
COPD can gradually get worse. How fast it progresses from mild to severe varies from person to person.
- Mild COPD (stage 1 or early stage). The first sign of COPD is often feeling out of breath with light exercises, like walking up stairs. Because it’s easy to blame this symptom on being out of shape or getting older, many people don’t realize they have COPD. Another sign is a phlegmy cough (a cough with mucus) that’s often particularly troublesome in the morning. These are early warning signs of COPD.
- Moderate to severe COPD (stages 2 and 3). In general, shortness of breath is more evident with more advanced COPD. You may develop shortness of breath even during everyday activities. Also, exacerbations of COPD, times when you experience increased phlegm, discoloration of phlegm, and more shortness of breath are generally more common in higher stages of COPD. You also become prone to lung infections like bronchitis and pneumonia.
- Very severe COPD (stage 4). When COPD becomes severe, almost everything you do can cause shortness of breath. This limits your mobility. You may need supplemental oxygen from a portable tank.
You can also read about types and stages of asthma
Risk factors of chronic obstructive pulmonary disease
Risk factors for COPD include:
- Exposure to tobacco smoke. The most significant risk factor for COPD is long-term cigarette smoking. The more years you smoke and the more packs you smoke, the greater your risk. Pipe smokers, cigar smokers and marijuana smokers also may be at risk, as well as people exposed to large amounts of secondhand smoke.
- People with asthma. Asthma, a chronic inflammatory airway disease, may be a risk factor for developing COPD. The combination of asthma and smoking increases the risk of COPD even more.
- Occupational exposure to dusts and chemicals. Long-term exposure to chemical fumes, vapors and dusts in the workplace can irritate and inflame your lungs.
- Exposure to fumes from burning fuel. In the developing world, people exposed to fumes from burning fuel for cooking and heating in poorly ventilated homes are at higher risk of developing COPD.
- Genetics. The uncommon genetic disorder alpha-1-antitrypsin deficiency is the cause of some cases of COPD. Other genetic factors likely make certain smokers more susceptible to the disease.
Complications of chronic obstructive pulmonary disease
As the disease progresses, you’re more susceptible to complications, such as:
- respiratory infections, including common colds, flu, and pneumonia
- heart problems
- high blood pressure in lung arteries (pulmonary hypertension)
- lung cancer
- depression and anxiety
You can also read about risk factors and complications of chronic cough
Prevention of chronic obstructive pulmonary disease
Unlike some diseases, COPD typically has a clear cause and a clear path of prevention, and there are ways to slow the progression of the disease. The majority of cases are directly related to cigarette smoking, and the best way to prevent COPD is to never smoke or to stop smoking now.
If you’re a longtime smoker, these simple statements may not seem so simple, especially if you’ve tried quitting once, twice or many times before. But keep trying to quit. It’s critical to find a tobacco cessation program that can help you quit for good. It’s your best chance for reducing damage to your lungs.
Occupational exposure to chemical fumes and dusts is another risk factor for COPD. If you work with these types of lung irritants, talk to your supervisor about the best ways to protect yourself, such as using respiratory protective equipment.
Here are some steps you can take to help prevent complications associated with COPD:
- Quit smoking to help reduce your risk of heart disease and lung cancer.
- Get an annual flu vaccination and regular vaccination against pneumococcal pneumonia to reduce your risk of or prevent some infections.
- Talk to your doctor if you feel sad or helpless or think that you may be experiencing depression.
Diagnosis of chronic obstructive pulmonary disease
To assess your lungs and overall health, your healthcare provider will take your medical history, perform a physical exam and order some tests, like breathing tests.
Medical history and physical exam
To diagnose COPD, your provider will ask questions like:
- Do you smoke?
- Have you had long-term exposure to dust or air pollutants?
- Do other members of your family have COPD?
- Do you get short of breath with exercise? When resting?
- Have you been coughing or wheezing for a long time?
- Do you cough up phlegm?
To help with the diagnosis, your provider will do a physical exam that includes:
- Listening to your lungs and heart.
- Checking your blood pressure and pulse.
- Examining your nose and throat.
- Checking your feet and ankles for swelling.
You can also read about prevention and diagnosis of pneumonia
Tests to diagnose COPD
Providers use a simple test called spirometry to see how well your lungs work. For this test, you blow air into a tube attached to a machine. This lung function test measures how much air you can breathe out and how fast you can do it. Your provider may also want to run a few other tests, such as:
- Pulse oximetry: This test measures the oxygen in your blood.
- Arterial blood gases (ABGs): These tests checkyour oxygen and carbon dioxide levels.
- Electrocardiogram (ECG or EKG): This test checks heart function and rules out heart disease as a cause of shortness of breath.
- Chest X-ray or chest CT scan: Imaging tests look for lung changes that COPD causes.
- Exercise testing: Your provider uses this to determine if the oxygen level in your blood drops when you exercise.
Treatment of chronic obstructive pulmonary disease
Many people with COPD have mild forms of the disease for which little therapy is needed other than smoking cessation. Even for more advanced stages of disease, effective therapy is available that can control symptoms, slow progression, reduce your risk of complications and exacerbations, and improve your ability to lead an active life.
The most essential step in any treatment plan for COPD is to quit all smoking. Stopping smoking can keep COPD from getting worse and reducing your ability to breathe. But quitting smoking isn’t easy. And this task may seem particularly daunting if you’ve tried to quit and have been unsuccessful.
Talk to your doctor about nicotine replacement products and medications that might help, as well as how to handle relapses. Your doctor may also recommend a support group for people who want to quit smoking. Also, avoid secondhand smoke exposure whenever possible.
Medications
Several kinds of medications are used to treat the symptoms and complications of COPD. You may take some medications on a regular basis and others as needed. These include:
- Bronchodilators
- Inhaled steroids
- Combination inhalers
- Oral steroids
- Phosphodiesterase-4 inhibitors
- Theophylline
- Antibiotics
Bronchodilators. Are medications that usually come in inhalers. They relax the muscles around your airways. This can help relieve coughing and shortness of breath and make breathing easier. Depending on the severity of your disease, you may need a short-acting bronchodilator before activities, a long-acting bronchodilator that you use every day or both.
Examples of short-acting bronchodilators include:
- Albuterol (ProAir HFA, Ventolin HFA, others)
- Ipratropium (Atrovent HFA)
- Levalbuterol (Xopenex)
Examples of long-acting bronchodilators include:
- Aclidinium (Tudorza Pressair)
- Arformoterol (Brovana)
- Formoterol (Perforomist)
- Indacaterol (Arcapta Neoinhaler)
- Tiotropium (Spiriva)
- Salmeterol (Serevent)
- Umeclidinium (Incruse Ellipta)
Inhaled corticosteroid medications. This can reduce airway inflammation and help prevent exacerbations. Side effects may include bruising, oral infections and hoarseness. These medications are useful for people with frequent exacerbations of COPD. Examples of inhaled steroids include:
- Fluticasone (Flovent HFA)
- Budesonide (Pulmicort Flexhaler)
Combination inhalers. Some medications combine bronchodilators and inhaled steroids. Examples of these combination inhalers include:
- Fluticasone and vilanterol (Breo Ellipta)
- Fluticasone, umeclidinium and vilanterol (Trelegy Ellipta)
- Formoterol and budesonide (Symbicort)
- Salmeterol and fluticasone (Advair HFA, AirDuo Digihaler, others)
Combination inhalers that include more than one type of bronchodilator also are available. Examples of these include:
- Aclidinium and formoterol (Duaklir Pressair)
- Albuterol and ipratropium (Combivent Respimat)
- Formoterol and glycopyrrolate (Bevespi Aerosphere)
- Glycopyrrolate and indacaterol (Utibron)
- Olodaterol and tiotropium (Stiolto Respimat)
- Umeclidinium and vilanterol (Anoro Ellipta)
Oral steroids. For people who experience periods when their COPD becomes more severe, called moderate or severe acute exacerbation, short courses (for example, five days) of oral corticosteroids may prevent further worsening of COPD. However, long-term use of these medications can have serious side effects, such as weight gain, diabetes, osteoporosis, cataracts and an increased risk of infection.
Phosphodiesterase-4 inhibitors. A medication approved for people with severe COPD and symptoms of chronic bronchitis is roflumilast (Daliresp), a phosphodiesterase-4 inhibitor. This drug decreases airway inflammation and relaxes the airways. Common side effects include diarrhea and weight loss.
Theophylline. When other treatment has been ineffective or if cost is a factor, theophylline (Elixophyllin, Theo-24, Theochron), a less expensive medication, may help improve breathing and prevent episodes of worsening COPD. Side effects are dose related and may include nausea, headache, fast heartbeat and tremor, so tests are used to monitor blood levels of the medication.
Antibiotics. Respiratory infections, such as acute bronchitis, pneumonia and influenza, can aggravate COPD symptoms. Antibiotics help treat episodes of worsening COPD, but they aren’t generally recommended for prevention. Some studies show that certain antibiotics, such as azithromycin (Zithromax), prevent episodes of worsening COPD, but side effects and antibiotic resistance may limit their use.
Lung therapies
Doctors often use these additional therapies for people with moderate or severe COPD:
- Oxygen therapy. If there isn’t enough oxygen in your blood, you may need supplemental oxygen. There are several devices that deliver oxygen to your lungs, including lightweight, portable units that you can take with you to run errands and get around town.Some people with COPD use oxygen only during activities or while sleeping. Others use oxygen all the time. Oxygen therapy can improve quality of life and is the only COPD therapy proved to extend life. Talk to your doctor about your needs and options.
- Pulmonary rehabilitation program.These programs generally combine education, exercise training, nutrition advice and counseling. You’ll work with a variety of specialists, who can tailor your rehabilitation program to meet your needs.Pulmonary rehabilitation after episodes of worsening COPD may reduce readmission to the hospital, increase your ability to participate in everyday activities and improve your quality of life. Talk to your doctor about referral to a program.
In-home noninvasive ventilation therapy
Evidence supports in-hospital use of breathing devices such as bilevel positive airway pressure (BiPAP), but some research now supports the benefit of its use at home. A noninvasive ventilation therapy machine with a mask helps to improve breathing and decrease retention of carbon dioxide (hypercapnia) that may lead to acute respiratory failure and hospitalization. More research is needed to determine the best ways to use this therapy.
Managing exacerbations
Even with ongoing treatment, you may experience times when symptoms become worse for days or weeks. This is called an acute exacerbation, and it may lead to lung failure if you don’t receive prompt treatment.
Exacerbations may be caused by a respiratory infection, air pollution or other triggers of inflammation. Whatever the cause, it’s important to seek prompt medical help if you notice a sustained increase in coughing or a change in your mucus, or if you have a harder time breathing.
When exacerbations occur, you may need additional medications (such as antibiotics, steroids or both), supplemental oxygen or treatment in the hospital. Once symptoms improve, your doctor can talk with you about measures to prevent future exacerbations, such as quitting smoking; taking inhaled steroids, long-acting bronchodilators or other medications; getting your annual flu vaccine; and avoiding air pollution whenever possible.
Surgery and medical procedure
Surgery is an option for some people with some forms of severe emphysema who aren’t helped sufficiently by medications alone. Surgical options include:
- Lung volume reduction surgery. In this surgery, your surgeon removes small wedges of damaged lung tissue from the upper lungs. This creates extra space in your chest cavity so that the remaining healthier lung tissue can expand and the diaphragm can work more efficiently. In some people, this surgery can improve quality of life and prolong survival. Endoscopic lung volume reduction is a minimally invasive procedure has recently been approved by the U.S. Food and Drug Administration to treat people with COPD. A tiny one-way endobronchial valve is placed in the lung, allowing the most damaged lobe to shrink so that the healthier part of the lung has more space to expand and function.
- Lung transplant. Lung transplantation may be an option for certain people who meet specific criteria. Transplantation can improve your ability to breathe and to be active. However, it’s a major operation that has significant risks, such as organ rejection, and you’ll need to take lifelong immune-suppressing medications.
- Bullectomy. Large air spaces (bullae) form in the lungs when the walls of the air sacs (alveoli) are destroyed. These bullae can become very large and cause breathing problems. In a bullectomy, doctors remove bullae from the lungs to help improve air flow.
Chronic obstructive pulmonary disease (COPD) causes lung damage that you can’t reverse. However, you can learn to manage symptoms. You’ll breathe easier if you take the necessary steps to support your lung capacity and fight lung irritation. By getting treatment early, you’ll have the best chance of continuing to do the things you love.
- List of Common Diseases & Medical Disorders
- Buy Complete Premium Anatomy Notes (PDFs)
- Medmichihealthcare New posts
- Read All causes of disease short notes
- Read All diagnosis of disease short notes
- Read All treatment of disease short notes
- Subscribe Medmichihealthcare YouTube channel
Discover more from Medmichihealthcare
Subscribe to get the latest posts sent to your email.