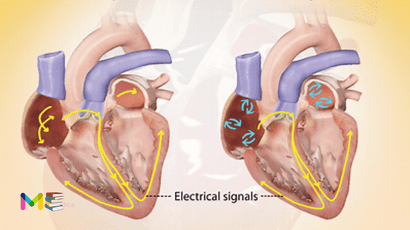
Atrial fibrillation (AFib) is an irregular and often very rapid heart rhythm. It can lead to blood clots in the heart. This condition also increases the risk of stroke, heart failure and other heart-related complications. It is one of the most common arrhythmias
During atrial fibrillation, the heart’s upper chambers called the atria, beat chaotically and irregularly. They beat out of sync with the lower heart chambers, called the ventricles. For many people, AFib may have no symptoms. But AFib may cause a fast, pounding heartbeat, shortness of breath or light-headedness.
The episodes of this condition may come and go, or they may be persistent. AFib itself usually isn’t life-threatening. But it’s a serious medical condition that needs proper treatment to prevent stroke. If left untreated, AFib can be deadly.
A person with atrial fibrillation also may have a related heart rhythm problem called atrial flutter. But the treatments for AFib and atrial flutter are similar.
Table of Contents
Types of atrial fibrillation
The following are the 4 main types of AFib:
- Paroxysmal Afib. This lasts less than one week and usually stops on its own without treatment.
- Persistent Afib. This lasts more than one week and needs treatment.
- Long-standing persistent Afib. This lasts more than a year and is sometimes difficult to treat.
- Permanent AFib. In this type of atrial fibrillation, the irregular heart rhythm can’t be reset. Medicines are needed to control the heart rate and to prevent blood clots.
Types and symptoms of heart murmurs
Symptoms of atrial fibrillation
The symptoms can come and go based on the severity of the condition. Some common symptoms of atrial fibrillation include:
- heart palpitations
- chest pain
- fatigue
- shortness of breath
- weakness
- lightheadedness
- dizziness
- fainting
- confusion
- intolerance to exercise
What’s the difference between a healthy and irregular heartbeat? An irregular heartbeat may be too fast, too slow, or inconsistent.
The average heart rate for a healthy person over age 10 is between 60 and 100 beats per minute. If your heart rate climbs higher or drops lower, this may be a sign of an irregular heartbeat.
You may also have the sensation that your heart is skipping a beat, fluttering, or beating too hard. These sensations are known as palpitations
Symptoms and causes of heart attack
Causes of atrial fibrillation
Problems with the heart’s structure are the most common cause of AFib. Heart diseases and health problems that can cause it include:
- A heart problem you’re born with, called a congenital heart defect.
- A problem with the heart’s natural pacemaker, called sick sinus syndrome.
- A sleep disorder called obstructive sleep apnea.
- Heart attack
- Heart valve disease.
- High blood pressure
- Lung diseases, including pneumonia
- Narrowed or blocked arteries, called coronary artery disease.
- Thyroid disease such as an overactive thyroid.
- Infections from viruses.
- Heart surgery or stress due to surgery or sickness may also cause it. Some people who have atrial fibrillation have no known heart disease or heart damage.
Lifestyle habits that can also trigger an AFib episode may include:
- Drinking too much alcohol or caffeine.
- Illegal drug use.
- Smoking or using tobacco.
- Taking medicines that contain stimulants, including cold and allergy medicines bought without a prescription.
Causes and risk factors of heart failure
Risk factors of atrial fibrillation
Some factors may put you at a higher risk for AFib. Some of these can be prevented, while others are genetic. These include:
- increased age (the older you are, the higher your risk)
- being white
- being male
- a family history of atrial fibrillation
- heart disease
- structural heart defects
- congenital heart defects
- pericarditis
- history of heart attacks
- history of heart surgery
- thyroid conditions
- metabolic syndrome
- obesity
- lung disease
- diabetes
- drinking alcohol, especially binge drinking
- sleep apnea
- high-dose steroid therapy
Risk factors and complications of high blood pressure
Complications of atrial fibrillation
Blood clots are a dangerous complication of AFib. Blood clots can lead to stroke. The risk of stroke from AFib increases as you grow older. Other health conditions also may increase the risk of a stroke due to AFib. These conditions include:
- High blood pressure
- Diabetes
- Heart failure.
- Some types of heart valve disease.
Blood thinners are commonly prescribed to prevent blood clots and strokes in people with this condition.
Prevention of atrial fibrillation
The following are the tips to lower the risk of atrial fibrillation:
- Follow a heart-healthy diet.
- Add aerobic exercise to your routine. Try for at least 150 minutes per week. Learn the target heart rate for your age and monitor your heart rate throughout exercise. Be sure to talk with your provider before starting any exercise plan.
- Limit your alcohol consumption.
- Quit smoking and using tobacco products. It can be hard to do this alone. With the right resources and support, you can achieve this goal and make your heart healthier.
- Control high blood pressure, high cholesterol and diabetes
- Get good sleep. Adults should aim for 7 to 9 hours daily.
- Maintain a healthy weight.
- Reduce and manage stress.
As you lower these risk factors, you will also see other benefits like reduced blood pressure, lower cholesterol levels and weight loss. When it comes to heart health, each positive lifestyle change has a ripple effect. The more changes you can make, the more benefits you will enjoy in the long run.
Prevention and diagnosis of stroke
Diagnosis of atrial fibrillation
Several different tests can be done to get a better idea of what’s going on with your heart function. A doctor may use one or more of the following tests to diagnose atrial fibrillation:
- A physical exam. This is to check your pulse, blood pressure, and lungs
- An electrocardiogram (EKG). This is a test that records the electrical impulses of your heart for a few seconds
If AFib doesn’t occur during the EKG, a doctor may have you wear a portable EKG monitor or try another type of test. These include:
- Holter monitor. A small portable device you wear for 24 to 48 hours to monitor your heart
- Event monitor. A device that records your heart only at certain times or when you’re having symptoms of AFib
- Echocardiogram. A noninvasive test that uses sound waves to produce a moving image of your heart
- Transesophageal echocardiogram. This is an invasive version of an echocardiogram that’s performed by placing a probe in the esophagus
- Stress test. This monitors your heart during exercise
- Chest X-ray. This is used to view your heart and lungs
- Blood tests. This is to check for thyroid and metabolic conditions
Treatment of atrial fibrillation
The goals of AFib treatment are to reset and control the heartbeat and prevent blood clots. Treatment depends on:
- How long you’ve had AFib.
- Your symptoms.
- The cause of the irregular heartbeat.
The treatment of this condition may involve:
- Medicine.
- Therapy to reset the heart rhythm, called cardioversion.
- Surgery or catheter procedures.
Together, you and your health care team discuss the best treatment option for you. It’s important to follow your atrial fibrillation treatment plan. If AFib isn’t well controlled, it may lead to other complications, including stroke and heart failure
Treatment for AFib may include medicines to do the following:
- Control the speed of the heartbeat.
- Restore the heart rhythm.
- Prevent blood clots, a dangerous complication of AFib.
Medicines that may be used include:
- Beta blockers. These medicines help slow the heart rate.
- Calcium channel blockers. These medicines control the heart rate but may need to be avoided by those who have heart failure or low blood pressure.
- Digoxin. This medicine may control the heart rate at rest, but not as well during activity. Most people need additional or alternative medicines, such as calcium channel blockers or beta blockers.
- Medicines to control the heart rate and rhythm. Also called anti-arrhythmics, this type of medicine is used sparingly. They tend to have more side effects than other medicines to control the heart rate.
- Blood thinners. Also called anticoagulants, these medicines help prevent blood clots and reduce the risk of stroke. Blood thinners include warfarin (Jantoven), apixaban (Eliquis), dabigatran (Pradaxa), edoxaban (Savaysa) and rivaroxaban (Xarelto). If you take warfarin, you’ll need to have regular blood tests to monitor the medicine’s effects.
If atrial fibrillation symptoms are bothersome or if this is the first AFib episode, a doctor may try to reset the heart rhythm using a procedure called cardioversion. Cardioversion can be done in two ways:
- Electrical cardioversion. This method to reset the heart rhythm is done by sending electric shocks to the heart through paddles or patches placed on the chest.
- Drug cardioversion. Medicines given through an IV or by mouth are used to reset the heart rhythm.
Cardioversion is usually done in a hospital as a scheduled procedure. However, it may be done in emergency situations. If it’s scheduled, a blood thinner such as warfarin (Jantoven) may need to be taken for a few weeks before the procedure. The medicine reduces the risk of blood clots and strokes.
After electrical cardioversion, medicines to control the heart rhythm may be needed for life to prevent future episodes of atrial fibrillation. Even with medicine, AFib could return.
Medical procedures
If AFib doesn’t get better with medicine or other treatments, a procedure called cardiac ablation may be necessary. Sometimes ablation is the first treatment.
Cardiac ablation uses heat or cold energy to create tiny scars in the heart. The scars disrupt irregular heart signals and restore a typical heartbeat. A doctor inserts a flexible tube called a catheter through a blood vessel, usually in your groin, and into your heart. More than one catheter may be used. Sensors on the tip of the catheter apply the cold or heat energy.
Less commonly, ablation is done using a scalpel during open-heart surgery.
There are several types of cardiac ablation. The type used to treat atrial fibrillation depends on your specific symptoms, overall health and whether you’re having another heart surgery. These include:
- Atrioventricular (AV) node ablation. Heat energy is usually applied to the heart tissue at the AV node to destroy the electrical signaling connection. After this treatment, a pacemaker is needed for life.
- Maze procedure. A doctor uses heat or cold energy or a scalpel to create a pattern or maze of scar tissue in the upper chambers of the heart. Scar tissue doesn’t send electrical signals. So the maze interferes with the stray heart signals that cause atrial fibrillation. If a scalpel is used to create the maze pattern, open-heart surgery is necessary. This is called the surgical maze procedure. It’s the preferred AFib treatment in those who need another heart surgery, such as coronary artery bypass surgery or heart valve repair.
- Hybrid atrial fibrillation ablation. This therapy combines ablation with surgery. It is used to treat long-standing persistent atrial fibrillation.
Atrial fibrillation may return after cardiac ablation. If this happens, another ablation or heart treatment may be recommended. After cardiac ablation, lifelong blood thinners may be needed to prevent strokes.
If you have AFib but can’t take blood thinners, you may need a procedure to seal a small sac in the left upper heart chamber. This sac, called an appendage, is where most AFibrelated clots form. This procedure is called left atrial appendage closure. A closure device is gently guided through a catheter to the sac. Once the device is in place, the catheter is removed. The device stays in permanently. Surgery to close the left atrial appendage also is an option for some people with AFib who are having another heart surgery.
- List of Common Diseases & Medical Disorders
- Buy Complete Premium Anatomy Notes (PDFs)
- Medmichihealthcare New posts
- Read All causes of disease short notes
- Read All diagnosis of disease short notes
- Read All treatment of disease short notes
- Subscribe Medmichihealthcare YouTube channel
Discover more from Medmichihealthcare
Subscribe to get the latest posts sent to your email.