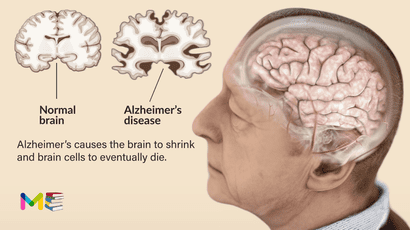
Alzheimer’s disease is a disorder of the brain that gets worse over time. It is a condition characterized by changes in the brain that lead to deposits or buildup of certain proteins. Alzheimer’s causes the brain to shrink and brain cells to eventually die. When this happens, it causes a gradual decline in memory, thinking, behavior and social skills. It’s the most common cause of dementia and usually affects people above the age of 65.
It is a common disease, and it affects approximately 24 million people across the world. One in 10 people older than 65 and nearly a third of people older than 85 have this disease. The symptoms of this condition worsen over time. Researchers believe the disease process may start 10 years or more before the first symptoms appear.
There’s no cure for Alzheimer’s yet, but there are treatments that can slow the progression of the disease. On average, a person with Alzheimer’s lives 4 to 8 years after diagnosis but can live as long as 20 years, depending on other factors. According to Alzheimer’s disease association
Table of Contents
Younger onset Alzheimer’s disease
Alzheimer’s typically affects people ages 65 and older. However, it can occur in people as early as in their 30s, 40s, or 50s. This is known as younger onset, or early onset Alzheimer’s. This type of Alzheimer’s affects fewer than 10% of all people with the condition, according to a research at National Institute of Aging
Stages of Alzheimer’s disease
This condition is a progressive disease, which simply means the symptoms will gradually increase with time. The following are the stages of Alzheimer’s:
Stages one to three (Pre-dementia and mild cognitive impairment)
- Stage 1. There are no symptoms at this stage. If you have a family history of Alzheimer’s and no symptoms, you may wish to talk to a doctor about strategies for healthy aging.
- Stage 2. The earliest symptoms appear, such as forgetfulness.
- Stage 3. Mild physical and cognitive impairments appear, such as reduced memory and concentration. Learning new skills may become harder. These changes may only be noticeable by someone very close to the person.
Stages four to seven (Dementia)
- Stage 4. Alzheimer’s is often diagnosed at this stage, but it’s still considered mild. It’s common to notice memory loss and to have difficulty managing everyday tasks.
- Stage 5. Moderate to severe symptoms will require help from loved ones or caregivers. This is necessary to ensure that daily needs are being met, such as eating meals and managing the home.
- Stage 6. At this stage, a person with Alzheimer’s will need help with basic tasks, such as eating, dressing, and toileting.
- Stage 7. This is the most severe and final stage of Alzheimer’s. There is usually a progressive loss of speech and facial expressions. Movement is likely to become limited.
As the stages of Alzheimer’s progress, those affected will need an increasing support from their caregivers.
Preclinical Alzheimer’s disease
Healthcare professionals typically only reference the preclinical stage in research on Alzheimer’s. People with this condition in the preclinical stage typically have no symptoms (are asymptomatic).
However, changes are taking place in their brain. This stage can last for years or even decades. People in this stage aren’t usually diagnosed with Alzheimer’s yet because they’re functioning at a high level.
According to new research, there’re now brain imaging tests that can detect deposits of a protein in your brain called amyloid that interfere with your brain’s communication system before symptoms start.
Symptoms of Alzheimer’s disease
The signs and symptoms of this disease vary depending on the stages. In general, the symptoms include a gradual decline in some, most or all of the following factors:
- Memory.
- Language.
- Reasoning and handling of complex tasks.
- Behavior and personality.
- Understanding visual form and space relationship.
Those with memory loss or other signs of Alzheimer’s can develop difficulty recognizing their mental decline. These signs may be more obvious to loved ones. Anyone experiencing dementia-like symptoms should see their doctor as early as possible.
Symptoms of Alzheimer’s with stages
Symptoms of Alzheimer’s become noticeable in the mild stage. The most common early symptom is forgetting newly learned information, especially recent events, places and names. Other signs and symptoms of mild stage include:
- Losing or misplacing objects more than usual.
- Having difficulty finding the right words to express thoughts.
- Having difficulty making plans or organizing.
- Taking longer to complete routine daily tasks.
- Having difficulty problem-solving.
Most people in the mild stage have no problem recognizing familiar faces and can usually travel to familiar places.
You can also read about when to seek help for memory loss
Moderate stage typically is the longest stage and can last many years. People in the moderate stage often require care and assistance. Those in this stage may:
- Have growing confusion about which day of the week it is, which season they’re in and where they are.
- Have increased memory loss and confusion, often forgetting events or details about their life, such as their telephone number or where they went to school.
- Have poor short-term memory.
- Have some difficulty recognizing friends and family.
- Repeat stories, thoughts or events that are on their minds.
- Have difficulty with simple math.
- Need help with self-care, such as bathing, grooming, showering and using the bathroom.
- Experience more personality changes, including being agitated or acting out. They may show depression, apathy or anxiety as the disease progresses.
- Develop groundless suspicions about family, friends and caregivers (delusions).
- Develop urinary incontinence and/or fecal (bowel) incontinence.
- Begin to wander from their living area.
- Have sleep disturbances.
In the final stage of Alzheimer’s, dementia symptoms are more severe. People in this stage need extensive care and monitoring. In the severe stage of this disease, people often:
- Is unaware of their surroundings.
- Has almost total memory loss.
- Loses their ability to communicate. Their speech becomes limited to a few words or phrases.
- Becomes vulnerable to infections, especially pneumonia and skin infections.
- Needs help with all basic activities of everyday living, such as eating, sitting up and walking.
You can also read the types and symptoms of stroke
Causes of Alzheimer’s disease
The exact causes of Alzheimer’s aren’t fully understood. But at a basic level, when brain proteins fail to function as usual, or when there’s abnormal build-up of proteins in your brain, this disrupts the work of brain cells, also called neurons, and triggers a series of events. The neurons become damaged and lose connections to each other, eventually they die.
Medical researchers believe that for most people, Alzheimer’s is caused by a combination of genetic, lifestyle and environmental factors that affect the brain over time. In less than 1% of cases, Alzheimer’s is caused by specific genetic changes that almost guarantee a person will develop the disease. In these cases, the disease usually begins in middle age.
The gradual development of this disorder begins years before the first symptoms. The damage most often starts in the region of the brain that controls memory. The loss of neurons spreads in a somewhat predictable pattern to other regions of the brain. By the late stage of the disease, the brain has shrunk significantly.
Medical researchers trying to understand the cause of Alzheimer’s are focused on the role of two proteins:
- Tangles. Tau proteins play a part in a brain cell’s internal support and transport system to carry nutrients and other essential materials. In Alzheimer’s disease, tau proteins change shape and organize into structures called neurofibrillary tangles. The tangles disrupt the transport system and cause damage to cells.
- Plaques. Beta-amyloid is a fragment of a larger protein. When these fragments clump together, they appear to have a toxic effect on neurons and to disrupt communication between brain cells. These clumps form larger deposits called amyloid plaques, which also include other cellular debris.
Risk factors of Alzheimer’s disease
Healthcare professionals have identified certain risk factors that contribute to Alzheimer’s, this may include:
- Age. Most people who develop Alzheimer’s disease are 65 years of age or older.
- Genetics. Certain genes have been linked to Alzheimer’s disease.
- Family history. If you have an immediate family member who has developed the condition, you’re more likely to get it.
Other possible risk factors of Alzheimer’s may include:
- depression
- Lifestyle (lack of exercise and obesity)
- smoking and alcohol
- cardiovascular disease
- Down syndrome
- High blood pressure
- High cholesterol
- Diabetes
- Mild cognitive impairment
- previous traumatic brain injury
These factors can all be modified. Changing lifestyle habits to some degree can alter the risk of Alzheimer’s. Regular exercise and a healthy low-fat diet rich in fruits and vegetables are related to lower the risk.
You can also read about causes and risk factors of high blood pressure
Complications of Alzheimer’s disease
The symptoms of Alzheimer’s such as memory loss, language loss, impaired judgment and other brain changes can make it very difficult to manage other health problems. People with this disease may not be able to:
- Explain symptoms of another illness.
- Tell someone about being in pain.
- Explain medicine side effects.
- Follow a treatment plan.
As the symptoms of Alzheimer’s progress to the last stages, brain changes begin to affect physical functions. This changes can affect the ability to swallow, balance, and control bowel and bladder movements. These can also lead to other health conditions such as:
- Falls.
- Fractures.
- Poor nutrition or dehydration.
- Inhaling food or liquid into the lungs.
- Flu, pneumonia and other infections.
- Constipation or diarrhea.
- Dental problems such as mouth sores or tooth decay.
- Bedsores.
Prevention of Alzheimer’s disease
There’s no known best ways to prevent this condition, but there’re some lifestyle changes that can help slow down cognitive decline. These may include:
- Eating well. Eat a balanced diet with plenty of fruits and vegetables.
- Exercising regularly. Getting active reduces the risk of many conditions, such as cardiovascular disease and diabetes.
- Keeping your brain active. Try some cognitive training exercises.
- Maintaining an active social life. Friendships, volunteering, and hobbies are likely to benefit your overall health.
- Quit smoking and alcohol. If you smoke, quitting benefits your health both immediately and in the long term.
You can discuss with your healthcare provider, other lifestyle changes that can help you with this condition.
You can also read about complications and prevention of diabetes
Diagnosis of Alzheimer’s disease
Healthcare professionals will try several methods to confirm if a person with memory issues has Alzheimer’s disease. This is because, there’re many other health problems, especially neurological conditions, that can also cause dementia and other symptoms of Alzheimer’s.
Diagnosing Alzheimer’s, your doctor will ask questions to better understand your health and daily living. Your doctor may also ask someone close to you, like a family member or caregiver, for insight into those symptoms you are having. Your healthcare provider will ask about:
- Your overall health.
- Your current medications.
- Your medical history.
- Your ability to carry out daily activities.
- Your changes in mood, behavior and personality.
Your healthcare provider will also do the following tests:
- Physical and neurological exam. Your healthcare provider will perform a physical exam and a neurological exam which may include testing Reflexes, Muscle tone and strength, Ability to get up from a chair and walk across the room, Sense of sight and hearing, Coordination and Balance.
- Lab tests. Blood tests may help rule out other potential causes of memory loss and confusion, such as a thyroid disorder or vitamin levels that are too low. Blood tests also can measure levels of beta-amyloid protein and tau protein, but these tests aren’t widely available and coverage may be limited.
- Mental status and neuropsychological testing. Your healthcare professional may give you a brief mental status test to assess memory and other thinking skills. Longer forms of this type of test may provide more details about mental function that can be compared with people of a similar age and education level. These tests can help establish a diagnosis and serve as a starting point to track symptoms in the future.
- Brain imaging. Images of the brain are typically used to pinpoint visible changes related to conditions other than Alzheimer’s disease that may cause similar symptoms, such as strokes, trauma or tumors. New imaging techniques may help detect specific brain changes caused by Alzheimer’s, but they’re used mainly in major medical centers or in clinical trials. Imaging of brain structures includes, Magnetic resonance imaging (MRI) and Computerized tomography (CT).
In some situations, other tests may be used to measure amyloid and tau in the cerebrospinal fluid. This can be done if symptoms are quickly getting worse or if dementia is affecting someone at a younger age (Younger onset Alzheimer’s disease) than what’s typical.
Medical researchers are finding a way to develop tests that can help measure biological signs of disease processes in the brain. These tests, including blood tests, might improve accuracy when performing a diagnosis. They can also allow the disease to be diagnosed before symptoms begin. A blood test to measure beta-amyloid levels is currently available.
Treatment of Alzheimer’s disease
As there’s no cure for Alzheimer’s, certain medications can temporarily slow the worsening of dementia symptoms and help with cognitive decline. Some medications and other interventions can also help with behavioral signs and symptoms.
The management of Alzheimer’s involve starting the treatment as early as possible, this could help maintain daily functioning for a while. However, current medications won’t stop or reverse the effect of Alzheimer’s.
As this disease affects everyone differently, the treatment plan is highly individualized. Healthcare professionals work with people with Alzheimer’s and their supportive caregivers to determine the best treatment plan that works.
The FDA approved two types of drugs to treat the symptoms of Alzheimer’s, which include:
- Cholinesterase inhibitors. Donepezil, Rivastigmine and Galantamine. These cholinesterase inhibitors can help treat the symptoms of mild to moderate Alzheimer’s disease. These drugs work by blocking the action of acetylcholinesterase, the enzyme responsible for destroying acetylcholine. Acetylcholine is one of the chemicals that help nerve cells communicate. Researchers believe that reduced levels of acetylcholine cause some of the symptoms of Alzheimer’s. These drugs can improve some memory problems and reduce some behavioral symptoms of Alzheimer’s. These medications don’t cure Alzheimer’s or stop the progression of the disease.
- NMDA antagonists. Memantine (Namenda) is FDA-approved for treating moderate to severe Alzheimer’s disease. It helps keep certain brain cells healthier. Studies have shown that people with Alzheimer’s who take memantine perform better in common activities of daily living such as eating, walking, toileting, bathing and dressing.
The FDA has also given accelerated approval for aducanumab (Aduhelm), the first disease-modifying therapy for Alzheimer’s. The medication helps to reduce amyloid deposits in your brain. Aducanumab is a new medication, and researchers studied its effects in people living with early Alzheimer’s. Because of this, it may only help people in the early stage.
In 2023, FDA approved lecanemab (Leqembi) for people with mild Alzheimer’s disease and mild cognitive impairment due to Alzheimer’s.
A phase 3 clinical trial found that the medicine slowed cognitive decline in people with early Alzheimer’s. The medicine prevents amyloid plaques in the brain from clumping. The phase 3 trial was the largest so far to study whether clearing clumps of amyloid plaques from the brain can slow the disease. Learn more about FDA approval of lecanemab
Managing behavior changes and Creating a safe and supportive environment for Alzheimer’s patients.
If you have a loved one diagnosed with Alzheimer’s, you can take the following steps to keep them comfortable in their environment and help their behavioral changes. You can:
- Monitor their comfort.
- Maintain a familiar environment for them. Don’t change the layout or organization of their living space.
- Provide comfort objects, such as a favorite stuffed animal or blanket.
- Try to avoid confrontation.
- Try to redirect their attention if they’re under stress.
There’s no medication yet, that has been approved for the management of behavioral symptoms in Alzheimer’s dementia patients. But certain medications may help in some people, these includes:
- Anti-anxiety drugs. These medications can treat agitation.
- Antidepressants. These drugs can treat anxiety, restlessness, aggression and depression.
- Antipsychotics (neuroleptics). These drugs can treat paranoia, hallucinations and agitation.
- Anticonvulsant drugs. These medications can sometimes treat aggression.
The above medications can cause unpleasant or potentially dangerous side effects (like dizziness, which could lead to falls). Healthcare professionals typically only prescribed them for short periods of time when behavioral problems are severe. Or after trying a safer non-drug therapies first. You can discuss more with your healthcare provider, about side effects of medications and other treatment methods that are best for you or your loved ones. And those steps to take that can slow down cognitive decline.
Subscribe YouTube Channel
- Subscribe Medmichihealthcare YouTube channel
- List of Common Diseases & Medical Disorders
- Buy Complete Premium Anatomy Notes (PDFs)
- Medmichihealthcare New posts
- Read All causes of disease short notes
- Read All diagnosis of disease short notes
- Read All treatment of disease short notes
Discover more from Medmichihealthcare
Subscribe to get the latest posts sent to your email.