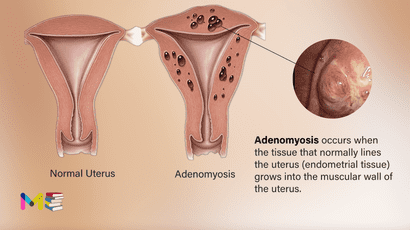
Adenomyosis occurs when the tissue that normally lines the uterus (endometrial tissue) grows into the muscular wall of the uterus. This condition makes the uterine walls thicker and distorts the vasculature (blood vessels), which can lead to heavy, prolonged, and painful periods. Adenomyosis is also associated with pain during sexual intercourse, as well as infertility.
Adenomyosis isn’t the same as endometriosis, which occurs when the endometrial lining grows outside of the uterus. People with adenomyosis may also have or develop endometriosis.
Many women and people assigned female at birth (AFAB) aren’t aware they have adenomyosis because the condition doesn’t always cause symptoms. The exact prevalence of adenomyosis is unknown. However, researchers know it’s more common in people who:
- Are older than 40.
- Have had a procedure on their uterus.
Approximately 2% to 5% of adolescents with severely painful cycles have adenomyosis.
Adenomyosis is believed to be estrogen-dependent or hormone-sensitive. It usually disappears after menopause, which takes place 12 months after a person’s final menstrual period. Menopause is also when estrogen levels decline.
Table of Contents
Symptoms of adenomyosis
Symptoms of this condition can be mild to severe. Some people may not experience any at all.
The most common symptoms include:
- heavy or prolonged menstrual bleeding
- painful menstrual cramps
- blood clots during menstrual bleeding
- pain during sexual intercourse
- infertility
Your uterus might get bigger. Although you might not know if your uterus is bigger, you may notice tenderness or pressure in your lower abdomen.
If you have prolonged, heavy bleeding or severe cramping during your periods that interferes with your regular activities, you should seek emergency medical attention immediately.
Causes of adenomyosis
The cause of adenomyosis isn’t well known. But there have been many theories that suggests the following:
- Invasive tissue growth. Some experts believe that endometrial cells from the lining of the uterus invade the muscle that forms the uterine walls.
- Developmental origins. Other experts suspect that endometrial tissue is deposited in the uterine muscle when the uterus is first formed in the fetus.
- Uterine inflammation related to childbirth. Another theory suggests a link between adenomyosis and childbirth. Inflammation of the uterine lining during the postpartum period might cause a break in the normal boundary of cells that line the uterus.
- Stem cell origins. A recent theory proposes that bone marrow stem cells might invade the uterine muscle, causing adenomyosis.
Regardless of how adenomyosis develops, its growth depends on the body’s circulating estrogen.
You can also read about the symptoms and causes of abnormal uterine bleeding
Risk factors of adenomyosis
There are certain factors that put people at greater risk for the condition. These include:
- age, with most people diagnosed in their 30s or 40s, a smaller proportion diagnosed as early as their teens, and some diagnosed after the age of 50 years old
- having given birth before
- undergoing treatment with the breast cancer drug tamoxifen
Other risk factors that have been suggested, but are controversial or have fewer data to support them, include:
- having had uterine surgery, like a cesarean delivery or surgery to remove uterine fibroids
- a history of depression or antidepressant use
- smoking
Complications of adenomyosis
Adenomyosis symptoms can negatively affect your lifestyle. Some people have excessive bleeding and pelvic pain that may prevent them from enjoying normal activities like sexual intercourse.
People with adenomyosis are at an increased risk of anemia, which is caused by blood loss and can result in an iron deficiency.
The blood loss associated with adenomyosis can reduce iron levels in the body. Without enough iron, the body can’t make enough red blood cells to carry oxygen to the body’s tissues. This can cause:
- Fatigue
- Dizziness
- Moodiness
Adenomyosis has also been linked with:
- Anxiety
- Depression
- Irritability
You can also read about risk factors and complications of preeclampsia
Prevention of adenomyosis
As the cause of adenomyosis isn’t well understood, healthcare providers don’t know of anything you can do to prevent it.
Diagnosis of adenomyosis
Healthcare providers often suspect adenomyosis based on your symptoms and one or more of these tests:
- Pelvic exam: During a pelvic exam, your provider may notice that your uterus has gotten larger, softer or is painful to the touch.
- Ultrasound: A transvaginal ultrasound uses sound waves to produce images of your pelvic organs. These images can sometimes show thickening of your uterine wall.
- Imaging scans: Magnetic resonance imaging (MRI) scans can show uterine enlargement and thickening of certain areas of your uterus.
Your provider may rule out more serious conditions with a biopsy. During a biopsy, your provider collects tissue and tests it for signs of more serious diseases.
You can also read about prevention and diagnosis of ectopic pregnancy
Treatment of adenomyosis
People with mild forms of adenomyosis may not require medical treatment. The doctor may recommend treatment options if your symptoms interfere with your daily activities or quality of life.
Treatments aimed at reducing the symptoms of adenomyosis include the following:
- Anti-inflammatory drugs. Your doctor might recommend anti-inflammatory medications, such as ibuprofen (Advil, Motrin IB, others), to control the pain. By starting an anti-inflammatory medicine one to two days before your period begins and taking it during your period, you can reduce menstrual blood flow and help relieve pain.
- Hormone medications. Combined estrogen-progestin birth control pills or hormone-containing patches or vaginal rings might lessen heavy bleeding and pain associated with adenomyosis. Progestin-only contraception, such as an intrauterine device, or continuous-use birth control pills often cause amenorrhea, the absence of your menstrual periods, which might provide some relief.
- Endometrial ablation: Endometrial ablation involves techniques to remove or destroy the endometrium. It’s an outpatient procedure with a short recovery time. But this procedure may not work for everyone, since adenomyosis often invades the muscle more deeply. It’s only recommended for people who have completed childbearing or aren’t interested in getting pregnant.
- Uterine artery embolization: Uterine artery embolization prevents certain arteries from supplying blood to the affected area. With the blood supply cut off, the adenomyoma shrinks. This procedure is typically used to treat uterine fibroids. The procedure is performed in a hospital. It usually involves staying overnight afterward. Since it’s minimally invasive, it doesn’t cause scar formation in the uterus.
- Ultrasound-guided focused ultrasound surgery: Ultrasound-guided focused ultrasound surgery uses precisely focused high-intensity waves to create heat and destroy the targeted tissue. The heat is monitored using ultrasound images in real-time. Early studies have shown this procedure to be effective in relieving symptoms. But more research is needed.
- Adenomyomectomy: Surgery to remove adenomyosis from your uterine muscle. This procedure is similar to a myomectomy, which removes uterine fibroids.
- Hysterectomy: The only way to completely cure adenomyosis is to have a hysterectomy, which involves the complete surgical removal of the uterus. It’s considered a major surgical intervention and is only used in severe cases and in people who don’t plan to give birth in the future. Your ovaries have no effect on adenomyosis. You and your doctor will have a discussion about whether there are other reasons to either remove them (especially if you’re postmenopausal) or leave them in place.
If adenomyosis is left untreated, adenomyosis can lead to infertility or miscarriage. This is because the embryo can’t implant into your uterine lining. Other problems may include chronic pelvic and abdominal pain.
You can also read about the treatment of oligohydramnios (amniotic fluid deficiency)
- List of Common Diseases & Medical Disorders
- Buy Complete Premium Anatomy Notes (PDFs)
- Medmichihealthcare New posts
- Read All causes of disease short notes
- Read All diagnosis of disease short notes
- Read All treatment of disease short notes
- Subscribe Medmichihealthcare YouTube channel
Discover more from Medmichihealthcare
Subscribe to get the latest posts sent to your email.