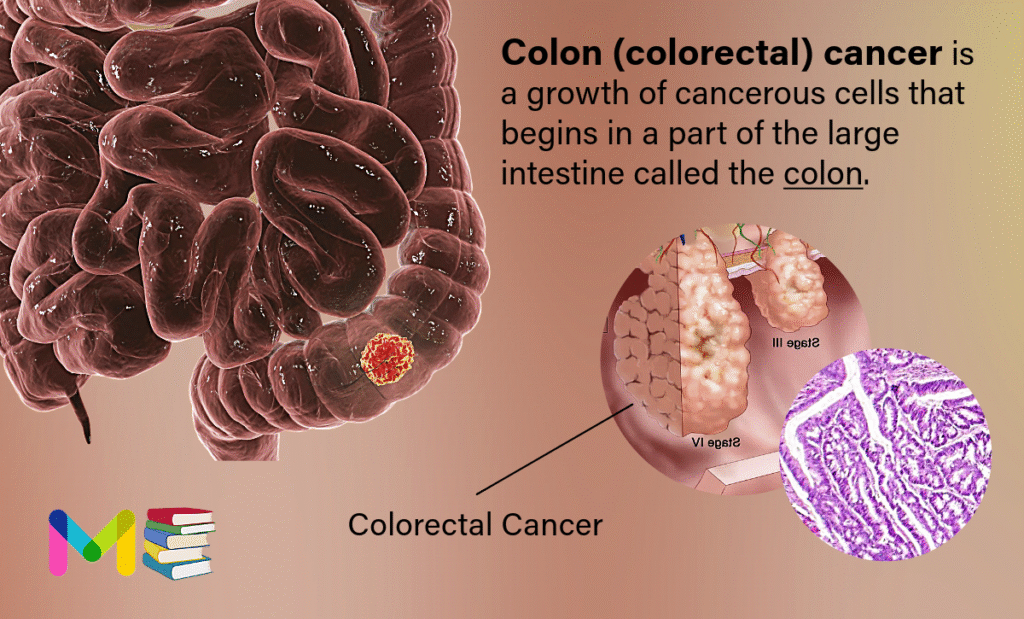
Colon (colorectal) cancer is a growth of cancerous cells that begins in a part of the large intestine called the colon. It’s often referred to as colorectal cancer. However, colorectal cancer is a group of cancers that includes both colon cancer and rectal cancer, which begins in the rectum.
Colon cancer typically affects people age 50 and older, though it can happen at any age. The American Cancer Society (ACS) estimates that about 1 in 24 males and 1 in 26 females will develop colorectal cancer during their lifetime.
Your colon is the long tube that helps carry digested food to your rectum and out of your body. Your colon wall is made of layers of mucous membrane, tissue and muscle. Colon cancer starts in your mucosa, the innermost lining of your colon. It consists of cells that make and release mucus and other fluids. If these cells mutate or change, they may create a colon polyp.
Over time, colon polyps may become cancerous. (It usually takes about 10 years for cancer to form in a colon polyp). Left undetected and/or untreated, the cancer works its way through a layer of tissue, muscle and the outer layer of your colon. It may also spread to other parts of your body via your lymph nodes or your blood vessels.
If colon cancer develops, many treatments can help control it. Treatments include surgery, radiation therapy and medicines, such as chemotherapy, targeted therapy and immunotherapy.
Table of Contents
Types of Colon Cancer
There are several types of colon cancer. They vary based on the different types of cancerous cells and where they’re located in the digestive tract.
The most common type of colon cancer starts from adenocarcinomas, according to the American Cancer Society (ACS). Adenocarcinomas in colon cancer form within the cells that make mucus in either the colon or rectum.
Less commonly, colon cancers are caused by other types of tumors, such as:
- lymphomas
- carcinoids
- sarcomas
- gastrointestinal stromal tumors
Stages of Colon Cancer
Healthcare providers use the TNM cancer staging system developed by the American Joint Committee on Cancer to stage colon cancer.
There are five stages of colon cancer. Three of the four stages have three sub-stages. The colon cancer staging system includes the following:
Stage 0: Healthcare providers may refer to this as carcinoma in situ. When they do, they’re talking about abnormal or precancerous cells in your mucosa, the innermost layer of your colon wall.
Stage I: Stage I colorectal cancer has grown into the wall of your intestine but hasn’t spread beyond the muscular coat or into close lymph nodes.
Stage II: The cancer has spread farther into the wall of your intestine but hasn’t spread to nearby lymph nodes. There are three types of Stage II colon cancer:
- Stage IIA: Cancer has spread through most of your colon wall but hasn’t grown into the wall’s outer layer.
- Stage IIB: Cancer has spread into the outer layer of your colon wall or through the wall.
- Stage IIC: Cancer has spread to a nearby organ.
Stage III: In this stage, colon cancer has spread to your lymph nodes. Like Stage II colon cancer, there are three sub-stages of Stage III colon cancer:
- Stage IIIA: There’s cancer in the first or second layers of your colon wall and it’s spread to one to four lymph nodes.
- Stage IIIB: The cancer affects more layers of your colon wall but only affects one to three lymph nodes. Cancer that affects fewer colon wall layers but has spread to four or more lymph nodes is also a stage IIIB colon cancer.
- Stage IIIC: There’s cancer in the outer layer or the next outermost layer of your colon and in four or more lymph nodes. Cancer that’s spread into a nearby organ and one or more lymph nodes is also a stage IIIC colon cancer.
Stage IV: Cancer has spread (metastasized) to other areas of your body, such as your liver, lungs or ovaries:
- Stage IVA: In this stage, cancer has spread to one organ or to lymph nodes that are farther or more distant from your colon.
- Stage IVB: The cancer has moved to more than one distant organ and more lymph nodes.
- Stage IVC: Cancer affects distant organs, lymph nodes and abdominal tissue.
You can also read: Types and Stages of Prostate Cancer
Symptoms of Colon Cancer
You might not experience colon cancer symptoms at all, especially in the early stages. If you do experience symptoms of colon cancer, they may include:
- constipation
- diarrhea
- blood in the stool
- changes in stool color
- changes in stool shape, such as narrowed stool
- bleeding from the rectum
- unintentional weight loss
- abdominal pain
- excessive fatigue
- the feeling that your bowel won’t completely empty (tenesmus)
It’s important to note that many of these symptoms may also be caused by other less serious conditions. It’s a good idea to see a doctor if you’ve had any of these symptoms for 3 weeks or more. You and the doctor can discuss your symptoms and decide if colon cancer screening is appropriate.
Causes of Colon Cancer
Medical researchers aren’t sure why some people develop precancerous colon polyps that become colon cancer. They do know certain risk factors increase people’s chances of developing precancerous polyps and colon cancer.
Like all types of cancer, colon cancer happens when cells grow and divide uncontrollably. All cells in your body are constantly growing, dividing and dying. That’s how your body remains healthy and working as it should. In colon cancer, when cells in the colon develop changes in their DNA. A cells’ DNA holds the instructions that tell the cell what to do. The changes tell the cells to multiply quickly. The changes let the cells continue living when healthy cells die as part of their natural lifecycle. This causes too many cells. The cells might form a mass called a tumor. The cells can invade and destroy healthy body tissue. In time, the cells can break away and spread to other parts of the body. When cancer spreads, it’s called metastatic cancer.
You can also read: Symptoms and Causes of Lung Cancer
Risk Factors of Colon Cancer
The risk factors of colon cancer include certain medical conditions, including inherited conditions, and lifestyle choices. Having one or more risk factors for colon cancer doesn’t mean you’ll develop the condition. It just means you have increased risk. Understanding risk factors may help you decide if you should talk to a healthcare provider about your risk of developing colon (colorectal) cancer.
Lifestyle choices that are risk factors for colon cancer
- Smoking: Using tobacco products, including chewing tobacco and e-cigarettes, increases your risk of developing colon cancer.
- Excessive alcohol use: In general, males should limit beverages containing alcohol to two servings a day. Females should limit beverages containing alcohol to one serving a day. Even light alcohol use can increase your risk of developing cancer.
- Having obesity: Eating high-fat, high-calorie foods may affect your weight and increase your risk of colon cancer.
- Having a diet that includes lots of red meat and processed meat: Processed meat includes bacon sausage and lunchmeat. Healthcare providers recommend you limit red meat and processed meat to two servings a week.
- Not exercising: Any kind of physical activity may reduce your risk of developing colon cancer.
Medical conditions that increase colon cancer risk
- Inflammatory bowel disease: People who have conditions like chronic ulcerative colitis and Crohn’s colitis, which cause inflammation in their colon lining, may have an increased risk of colon cancer. The risk increases if you have inflammatory bowel disease that lasts more than seven years and affects large parts of your colon.
- Inherited conditions: Certain conditions like Lynch syndrome and familial adenomatous polyposis may increase your risk of developing colon cancer. Colon cancer may happen if you inherit a gene that causes cancer.
- A family history of colon and other kinds of cancer: If a close family member has colon cancer, you may have an increased risk of developing the condition. Close family members include your biological parents, siblings and children. Your risk may be higher if any biological family member developed colon cancer before age 45.
- A family history of polyps: If your parent, sibling or child has an advanced polyp, you may have an increased risk of getting colon cancer. An advanced polyp may be a large polyp. Medical pathologists may characterize a polyp as being advanced if they see certain changes in the polyp when they look at it under a microscope that are signs the polyp may contain cancerous cells.
- Many polyps: People with numerous colon polyps — including adenomas, serrated polyps or other types of polyps — often have an increased risk of developing polyps and colon cancer. People may inherit a tendency toward having many colon polyps.
Prevention of Colon Cancer
Doctors recommend that people with an average risk of colon cancer consider starting colon cancer screening around age 45. But people with an increased risk should think about starting screening sooner. People with an increased risk include those with a family history of colon cancer.
There are several different tests that are used for colon cancer screening. Talk about your options with your health care team.
Making changes in everyday life can reduce the risk of colon cancer. To lower the risk of colon cancer:
- Eat a variety of fruits, vegetables and whole grains. Fruits, vegetables and whole grains have vitamins, minerals, fiber and antioxidants, which may help prevent cancer. Choose a variety of fruits and vegetables so that you get a range of vitamins and nutrients.
- Drink alcohol in moderation, if at all. If you choose to drink alcohol, limit the amount you drink to no more than one drink a day for women and two for men.
- Stop smoking. Talk to your health care team about ways to quit.
- Exercise most days of the week. Try to get at least 30 minutes of exercise on most days. If you’ve been inactive, start slowly and build up gradually to 30 minutes. Also, talk with a health care professional before starting an exercise program.
- Maintain a healthy weight. If you are at a healthy weight, work to maintain your weight by combining a healthy diet with daily exercise. If you need to lose weight, ask your health care team about healthy ways to achieve your goal. Aim to lose weight slowly by eating fewer calories and moving more.
Colon cancer prevention for people with a high risk
Some medicines can reduce the risk of colon polyps or colon cancer. For instance, some evidence links a reduced risk of polyps and colon cancer to regular use of aspirin or aspirin-like medicines. But it’s not clear what dose and what length of time would be needed to reduce the risk of colon cancer. Taking aspirin daily has some risks, including ulcers and bleeding in the digestive system.
These options are generally reserved for people with a high risk of colon cancer. There isn’t enough evidence to recommend these medicines to people who have an average risk of colon cancer.
If you have an increased risk of colon cancer, discuss your risk factors with your health care team to see if preventive medicines are safe for you.
You can also read: Risk Factors and Prevention of Leukemia
Diagnosis of Colon Cancer
Healthcare providers use several tests to diagnose colon cancer. Those tests include:
- Complete blood count (CBC).
- Comprehensive metabolic panel (CMP).
- Carcinoembryonic antigen (CEA) assay: Cancer cells and normal cells release CEA into your bloodstream. High CEA levels may be a sign of colon cancer.
- X-rays.
- Computed tomography (CT) scan.
- Magnetic resonance imaging (MRI) scan.
- Positron emission tomography (PET) scan.
- Ultrasound.
- Biopsy.
A cancer screening test checks for cancer when you don’t have any signs or symptoms of cancer. If your screening test shows abnormalities, a healthcare provider may recommend additional tests.
What are common colon cancer screening tests?
A colonoscopy is the most common screening test for colon cancer. Other tests include:
- Fecal immunochemical test (FIT): This test detects hidden blood in your poop. Medical pathologists test samples of your poop for blood that you may not see just by looking.
- Guaiac-based fecal occult blood test (gFOBT): Like the FIT, this test looks for blood in poop that may not be visible.
- Fecal DNA test: This test looks for signs of genetic mutations and blood products in your poop.
- Flexible sigmoidoscopy: Healthcare providers use a flexible scope called a sigmoidoscope to see inside your lower colon and rectum.
- Virtual colonoscopy: A virtual colonoscopy is an X-ray that looks for polyps, tumors and ulcers (sores) in your colon and rectum.
Treatment of Colon Cancer
Colon cancer treatment usually involves surgery to remove the cancer. Your health care team might recommend other treatments, such as radiation therapy and chemotherapy. Your treatment options depend on the cancer’s location and its stage. Your health care team also considers your overall health and your preferences when creating a treatment plan.
Surgery for early-stage colon cancer
Treatment for a very small colon cancer might be a minimally invasive approach to surgery, such as:
- Removing polyps during a colonoscopy, called a polypectomy. If the cancer is contained within a polyp, removing the polyp may remove all of the cancer.
- Endoscopic mucosal resection. This procedure can remove larger polyps during colonoscopy. Special tools help remove the polyp and a small amount of the lining of the colon.
- Minimally invasive surgery, called laparoscopic surgery. This type of surgery can remove polyps that can’t be removed during a colonoscopy. In this procedure, a surgeon performs the operation through several small cuts called incisions in the abdominal wall. Instruments with attached cameras go through the cuts and show the colon on a video monitor. The surgeon also may take samples from lymph nodes in the area around the cancer.
Surgery for more advanced colon cancer
If the cancer has grown into or through the colon, a surgeon might recommend:
- Partial colectomy. Surgery to remove part of the colon is called partial colectomy. During this procedure, the surgeon removes the part of the colon that has the cancer. The surgeon also takes some tissue on either side of the cancer. It’s often possible to reconnect the healthy portions of the colon or rectum. This procedure can often be done by a minimally invasive approach called laparoscopy.
- Surgery to create a way for waste to leave the body. Sometimes it’s not possible to reconnect the healthy portions of the colon or rectum after colectomy. The surgeon creates an opening in the wall of the abdomen from a portion of what’s left of the intestine. This procedure, called an ostomy, allows stool to leave the body by emptying into a bag that fits over the opening.Sometimes the ostomy is only for a short time to let the colon or rectum heal after surgery. Then it’s reversed. Sometimes the ostomy can’t be reversed and stays for life.
- Lymph node removal. Nearby lymph nodes are usually removed during colon cancer surgery and tested for cancer.
Surgery for advanced cancer
When it’s not possible to remove the cancer with surgery, a surgeon might try to relieve symptoms rather than cure the cancer. This surgery can remove colon blockages and ease symptoms, such as bleeding or pain.
Sometimes the cancer has spread only to the liver or lung in someone who is otherwise healthy. Surgery or other localized treatments might remove the cancer. Chemotherapy might be used before or after this type of procedure. This approach provides a chance to be free of cancer over the long term.
Chemotherapy
Chemotherapy uses strong medicines to kill cancer cells. Chemotherapy for colon cancer is usually given after surgery if the cancer is large or has spread to the lymph nodes. Chemotherapy can kill cancer cells that might be left after surgery. This helps reduce the risk of the cancer coming back.
Chemotherapy might also be used before surgery to shrink a large cancer so that it’s easier to remove.
Chemotherapy also can be used to relieve symptoms of colon cancer that can’t be removed with surgery or that has spread to other areas of the body. Sometimes it’s used with radiation therapy.
Radiation therapy
Radiation therapy uses powerful energy beams to kill cancer cells. The energy can come from X-rays, protons or other sources.
Radiation therapy can shrink a large cancer before an operation to make it easier to remove. When surgery isn’t an option, radiation therapy might be used to relieve symptoms, such as pain. Some people have radiation and chemotherapy at the same time.
Targeted therapy
Targeted therapy uses medicines that attack certain chemicals in cancer cells. By blocking these chemicals, targeted treatments can cause cancer cells to die.
Targeted therapy is usually combined with chemotherapy. Targeted therapy is typically used for people with advanced colon cancer.
Immunotherapy
Immunotherapy is a treatment with medicine that helps the body’s immune system kill cancer cells. The immune system fights off diseases by attacking germs and other cells that shouldn’t be in the body. Cancer cells survive by hiding from the immune system. Immunotherapy helps the immune system cells find and kill the cancer cells. Immunotherapy is usually reserved for advanced colon cancer.
You can also read: Diagnosis and Treatment of Hemophilia
Conclusion
The progression of colon cancer varies for each person. However, the American Cancer Society (ACS) notes that colon cancer usually takes years to develop and spread. Early detection and treatment are key to preventing further spreading and complications. If colon cancer is diagnosed in the early stages, surgery may be able to completely remove the cancerous polyp.
- List of Common Diseases & Medical Disorders
- Buy Complete Premium Anatomy Notes (PDFs)
- Medmichihealthcare New posts
- Read All causes of disease short notes
- Read All diagnosis of disease short notes
- Read All treatment of disease short notes
- Subscribe Medmichihealthcare YouTube channel
Discover more from Medmichihealthcare
Subscribe to get the latest posts sent to your email.