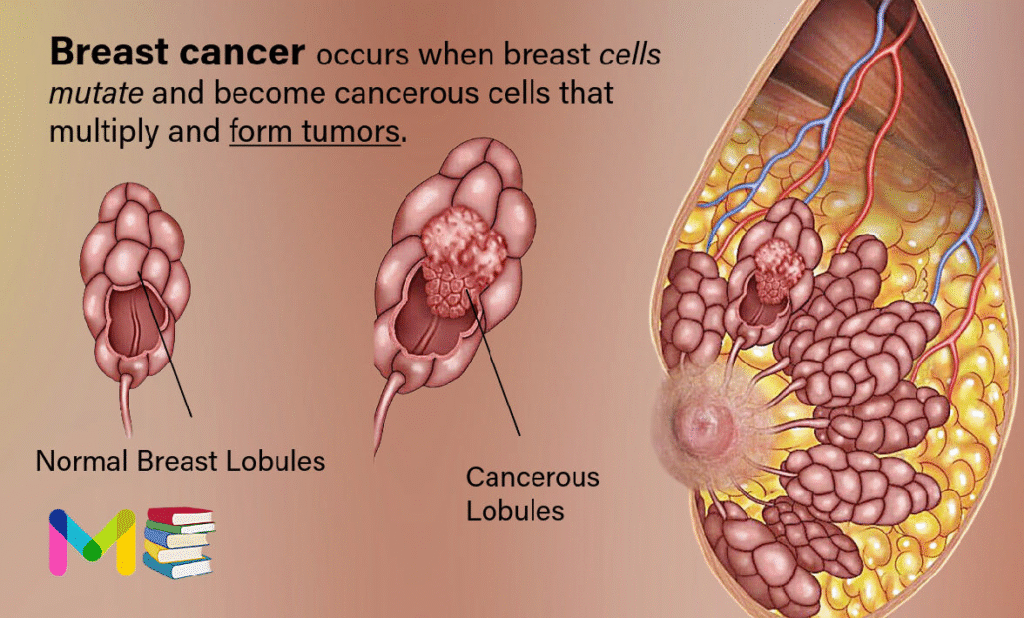
Breast cancer occurs when breast cells mutate and become cancerous cells that multiply and form tumors. Typically, the cancer forms in either the lobules or the ducts of the breast.
Lobules are the glands that produce milk, and ducts are the pathways that bring the milk from the glands to the nipple. Cancer can also occur in the fatty tissue or the fibrous connective tissue within your breast.
The uncontrolled cancer cells often invade other healthy breast tissue and can travel to the lymph nodes under the arms. Once the cancer enters the lymph nodes, it has access to a pathway to move to other body parts.
After skin cancer, breast cancer is one of the most common cancers that affects women. Breast cancer typically affects women aged 50 and older, but it can also affect men, as well as younger women. Healthcare providers may treat breast cancer with surgery to remove tumors or treatment to kill cancerous cells.
About 80% of breast cancer cases are invasive, meaning a tumor may spread from your breast to other areas of your body. People with breast cancer may first notice a lump in the breast, discoloration, texture changes, or other symptoms.
Breast cancer survival rates have been increasing. And the number of people dying of breast cancer is steadily going down. Much of this is due to the widespread support for breast cancer awareness and funding for research.
Advances in breast cancer screening allow healthcare professionals to diagnose breast cancer earlier. Finding the cancer earlier makes it much more likely that the cancer can be cured. Even when breast cancer can’t be cured, many treatments exist to extend life. New discoveries in breast cancer research are enabling healthcare professionals to select the most effective treatment plans.
Table of Contents
Types of breast cancer
Healthcare providers determine cancer types and subtypes so they can tailor treatment to be as effective as possible with the fewest possible side effects. Common types of breast cancer include:
- Invasive (infiltrating) ductal carcinoma (IDC): This cancer starts in your milk ducts and spreads to nearby breast tissue. It’s the most common type of breast cancer in the United States.
- Lobular breast cancer: This breast cancer starts in the milk-producing glands (lobules) in your breast and often spreads to nearby breast tissue. It’s the second most common breast cancer in the United States.
- Ductal carcinoma in situ (DCIS): Like IDC, this breast cancer starts in your milk ducts. The difference is DCIS doesn’t spread beyond your milk ducts.
Less common breast cancer types include:
- Triple-negative breast cancer (TNBC): This invasive cancer is aggressive and spreads more quickly than other breast cancers.
- Inflammatory breast cancer (IBC): This rare, fast-growing cancer looks like a rash on your breast. IBC is rare in the United States.
- Paget’s disease of the breast: This rare cancer affects the skin of your nipple and may look like a rash. Less than 4% of all breast cancers are Paget’s disease of the breast.
Breast cancer subtypes
Healthcare providers classify breast cancer subtypes by receptor cell status. Receptors are protein molecules in or on cells’ surfaces. They can attract or attach to certain substances in your blood, including hormones like estrogen and progesterone.
Estrogen and progesterone help cancerous cells to grow. Finding out if cancerous cells have estrogen or progesterone receptors helps healthcare providers plan breast cancer treatment.
Subtypes include:
- ER-positive (ER+) breast cancers have estrogen receptors.
- PR-positive (PR+) breast cancers have progesterone receptors.
- HR-positive (HR+) breast cancers have estrogen and progesterone receptors.
- HR-negative (HR-) breast cancers don’t have estrogen or progesterone receptors.
- HER2-positive (HER2+) breast cancers, which have higher than normal levels of the HER2 protein. This protein helps cancer cells to grow. About 15% to 20% of all breast cancers are HER2-positive.
Breast cancer stages
Doctors divide breast cancer into stages based on the size of the tumor and how much it has spread.
Cancers that are large or have invaded nearby tissues or organs are at a higher stage than cancers that are small or still contained in the breast.
To stage breast cancer, doctors need to know:
- if the cancer is invasive or noninvasive
- how large the tumor is
- whether the lymph nodes are involved
- if the cancer has spread to nearby tissue or organs
Breast cancer has five main stages: stages 0 to 4.
Stage 0 breast cancer
Stage 0 is ductal carcinoma in situ (DCIS). Cancer cells in DCIS remain confined to the ducts in the breast and have not spread into nearby tissue.
Stage 1 breast cancer
- Stage 1A: The primary tumor is 2 centimeters (cm) wide or less. The lymph nodes are not affected.
- Stage 1B: Cancer is found in nearby lymph nodes. Either there is no tumor in the breast, or the tumor is smaller than 2 cm.
Stage 2 breast cancer
- Stage 2A: The tumor is smaller than 2 cm and has spread to one to three nearby lymph nodes, or it’s between 2 and 5 cm and hasn’t spread to any lymph nodes.
- Stage 2B: The tumor is between 2 and 5 cm and has spread to one to three axillary (armpit) lymph nodes, or it’s larger than 5 cm and hasn’t spread to any lymph nodes.
Stage 3 breast cancer
- Stage 3A:
- The cancer has spread to four to nine axillary lymph nodes or has enlarged the internal mammary lymph nodes. The primary tumor can be any size.
- Tumors are greater than 5 cm. The cancer has spread to one to three axillary lymph nodes or any breastbone nodes.
- Stage 3B: A tumor has invaded the chest wall or skin and may or may not have invaded up to nine lymph nodes.
- Stage 3C: Cancer is found in 10 or more axillary lymph nodes, lymph nodes near the collarbone, or internal mammary nodes.
Stage 4 breast cancer (metastatic breast cancer)
Stage 4 breast cancer can have a tumor of any size. Its cancer cells have spread to nearby and distant lymph nodes as well as distant organs.
The testing a doctor does will determine the stage of your breast cancer, which will affect your treatment.
You can also read: Types & Stages of prostate cancer
Symptoms of breast cancer
In its early stages, breast cancer may not cause any symptoms. In many cases, a tumor may be too small to be felt, but an abnormality can still be seen on a mammogram.
If a tumor can be felt, the first sign is usually a new lump in the breast that was not there before. However, not all lumps are cancer.
Symptoms of the most common breast cancers include:
- a breast lump or tissue thickening that feels different from surrounding tissue and is new
- breast pain
- discolored and pitted skin on your breast
- swelling in all or part of your breast
- a nipple discharge other than breast milk
- bloody discharge from your nipple
- peeling, scaling, or flaking of skin on your nipple or breast
- a sudden, unexplained change in the shape or size of your breast
- inverted nipple
- changes to the appearance of the skin on your breasts
- a lump or swelling under your arm
If you have any of these symptoms, it doesn’t necessarily mean you have breast cancer. For instance, pain in your breast or a breast lump can be caused by a benign cyst.
Still, if you find a lump in your breast or have other symptoms, speak with a doctor for further examination and testing.
Causes of breast cancer
The exact cause of most breast cancers isn’t known. Researchers have found things that increase the risk of breast cancer. These include hormones, lifestyle choices and things in the environment. But it’s not clear why some people who don’t have any factors get cancer, yet others with risk factors never do. It’s likely that breast cancer happens through a complex interaction of your genetic makeup and the world around you.
Healthcare professionals know that breast cancer starts when something changes the DNA inside cells in the breast tissue. A cell’s DNA holds the instructions that tell a cell what to do. In healthy cells, the DNA gives instructions to grow and multiply at a set rate. The instructions tell the cells to die at a set time. In cancer cells, the DNA changes give different instructions. The changes tell the cancer cells to make many more cells quickly. Cancer cells can keep living when healthy cells would die. This causes too many cells.
The cancer cells might form a mass called a tumor. The tumor can grow to invade and destroy healthy body tissue. In time, cancer cells can break away and spread to other parts of the body. When cancer spreads, it’s called metastatic cancer.
The DNA changes that lead to breast cancer most often happen in the cells that line the milk ducts. These ducts are tubes designed to carry milk to the nipple. Breast cancer that starts in the ducts is called invasive ductal carcinoma. Breast cancer also can start in cells in the milk glands. These glands, called lobules, are designed to make breast milk. Cancer that happens in the lobules is called invasive lobular carcinoma. Other cells in the breast can become cancer cells, though this isn’t common.
You can also read: Symptoms & Causes of bladder cancer
Risk factors of breast cancer
Factors that may increase the risk of breast cancer include:
- A family history of breast cancer. If a parent, sibling or child had breast cancer, your risk of breast cancer is increased. The risk is higher if your family has a history of getting breast cancer at a young age. The risk also is higher if you have multiple family members with breast cancer. Still, most people diagnosed with breast cancer don’t have a family history of the disease.
- A personal history of breast cancer. If you’ve had cancer in one breast, you have an increased risk of getting cancer in the other breast.
- A personal history of breast conditions. Certain breast conditions are markers for a higher risk of breast cancer. These conditions include lobular carcinoma in situ, also called LCIS, and atypical hyperplasia of the breast. If you’ve had a breast biopsy that found one of these conditions, you have an increased risk of breast cancer.
- Beginning your period at a younger age. Beginning your period before age 12 increases your risk of breast cancer.
- Beginning menopause at an older age. Beginning menopause after age 55 increases the risk of breast cancer.
- Being female. Women are much more likely than men are to get breast cancer. Everyone is born with some breast tissue, so anyone can get breast cancer.
- Dense breast tissue. Breast tissue is made up of fatty tissue and dense tissue. Dense tissue is made of milk glands, milk ducts and fibrous tissue. If you have dense breasts, you have more dense tissue than fatty tissue in your breasts. Having dense breasts can make it harder to detect breast cancer on a mammogram. If a mammogram showed that you have dense breasts, your risk of breast cancer is increased. Talk with your healthcare team about other tests you might have in addition to mammograms to look for breast cancer.
- Drinking alcohol. Drinking alcohol increases the risk of breast cancer.
- Having your first child at an older age. Giving birth to your first child after age 30 may increase the risk of breast cancer.
- Having never been pregnant. Having been pregnant one or more times lowers the risk of breast cancer. Never having been pregnant increases the risk.
- Increasing age. The risk of breast cancer goes up as you get older.
- Inherited DNA changes that increase cancer risk. Certain DNA changes that increase the risk of breast cancer can be passed from parents to children. The most well-known changes are called BRCA1 and BRCA2. These changes can greatly increase your risk of breast cancer and other cancers, but not everyone with these DNA changes gets cancer.
- Menopausal hormone therapy. Taking certain hormone therapy medicines to control the symptoms of menopause may increase the risk of breast cancer. The risk is linked to hormone therapy medicines that combine estrogen and progesterone. The risk goes down when you stop taking these medicines.
- Obesity. People with obesity have an increased risk of breast cancer.
- Radiation exposure. If you received radiation treatments to your chest as a child or young adult, your risk of breast cancer is higher.
Complications of breast cancer
The most significant complication is metastatic breast cancer — breast cancer that spreads to other areas of your body, including your brain, bones, liver and lungs. Studies show about 1 in 3 women who have early-stage cancer later develop metastatic breast cancer.
You can also read: Risk factors & Complications of Colon cancer
Prevention of breast cancer
Things you can do to lower your risk of breast cancer. Making changes in your daily life may help lower your risk of breast cancer. Try to:
- Ask about breast cancer screening. Talk with your doctor or other healthcare professional about when to begin breast cancer screening. Ask about the benefits and risks of screening. Together, you can decide what breast cancer screening tests are right for you.
- Become familiar with your breasts through breast self-exam for breast awareness. You may choose to become familiar with your breasts by occasionally inspecting them during a breast self-exam for breast awareness. If there is a new change, a lump or something not typical in your breasts, report it to a healthcare professional right away.Breast awareness can’t prevent breast cancer. But it may help you to better understand the look and feel of your breasts. This might make it more likely that you’ll notice if something changes.
- Drink alcohol in moderation, if at all. Limit the amount of alcohol you drink to no more than one drink a day, if you choose to drink. For breast cancer prevention, there is no safe amount of alcohol. So if you’re very concerned about your breast cancer risk, you may choose to not drink alcohol.
- Exercise most days of the week. Aim for at least 30 minutes of exercise on most days of the week. If you haven’t been active lately, ask a healthcare professional whether it’s OK and start slowly.
- Limit menopausal hormone therapy. Combination hormone therapy may increase the risk of breast cancer. Talk with a healthcare professional about the benefits and risks of hormone therapy.Some people have symptoms during menopause that cause discomfort. These people may decide that the risks of hormone therapy are acceptable in order to get relief. To reduce the risk of breast cancer, use the lowest dose of hormone therapy possible for the shortest amount of time.
- Maintain a healthy weight. If your weight is healthy, work to maintain that weight. If you need to lose weight, ask a healthcare professional about healthy ways to lower your weight. Eat fewer calories and slowly increase the amount of exercise.
Medicines and operations for those with a high risk of breast cancer
If you have a high risk of breast cancer, you might consider other options to lower the risk. You might have a high risk if you have a family history of breast cancer. Your risk also might be higher if you have a history of precancerous cells in the breast tissue. Talk about your risk with your healthcare team. Your team might have options for lowering your risk, such as:
- Preventive medicines. Using estrogen-blocking medicines can lower the risk of breast cancer in those who have a high risk. Options include medicines called selective estrogen receptor modulators and aromatase inhibitors. These medicines also are used as hormone therapy treatment for breast cancer. These medicines carry a risk of side effects. For this reason, they’re only used in those who have a very high risk of breast cancer. Discuss the benefits and risks with your healthcare team.
- Preventive surgery. If you have a very high risk of breast cancer, you may consider having surgery to lower the risk of breast cancer. One option might be surgery to remove the breasts, called prophylactic mastectomy. Another option is surgery to remove the ovaries, called prophylactic oophorectomy. This operation lowers the risk of breast cancer and ovarian cancer.
Breast cancer screening
Having regular mammograms may not prevent breast cancer, but it can help reduce the chance that it will go undetected.
The American Cancer Society provides the following general recommendations for those at average risk of breast cancer:
- Ages 40 to 44 years: an optional mammogram each year
- Ages 45 to 54 years: a mammogram every year
- Ages 55 years and older: can choose to continue with annual mammograms or switch to every other year
Specific recommendations for mammograms are different for everyone, so talk with a doctor to see if you should get regular mammograms.
Breast cancer diagnosis
Healthcare providers may do physical examinations or order mammograms to check for signs of breast cancer. But they do the following tests to diagnose the disease:
- Breast ultrasound.
- Breast magnetic resonance imaging (MRI) scan.
- Breast biopsy.
- Immunohistochemistry test to check for hormone receptors.
- Genetic tests to identify mutations that cause breast cancer.
You can also read: Prevention & diagnosis of lung cancer
Treatment of breast cancer
Breast cancer treatment often starts with surgery to remove the cancer. Most people with breast cancer will have other treatments after surgery, such as radiation, chemotherapy and hormone therapy. Some people may have chemotherapy or hormone therapy before surgery. These medicines can help shrink the cancer and make it easier to remove.
Your treatment plan will depend on your particular breast cancer. Your healthcare team considers the stage of the cancer, how quickly it’s growing and whether the cancer cells are sensitive to hormones. Your care team also considers your overall health and what you prefer.
There are many options for breast cancer treatment. It can feel overwhelming to consider all the options and make complex decisions about your care. Consider seeking a second opinion from a breast specialist in a breast center or clinic. Talk to breast cancer survivors who have faced the same decision.
Breast cancer surgery
Breast cancer surgery typically involves a procedure to remove the breast cancer and a procedure to remove some nearby lymph nodes. Operations used to treat breast cancer include:
- Removing the breast cancer. A lumpectomy is surgery to remove the breast cancer and some of the healthy tissue around it. The rest of the breast tissue isn’t removed. Other names for this surgery are breast-conserving surgery and wide local excision. Most people who have a lumpectomy also have radiation therapy. Lumpectomy might be used to remove a small cancer. Sometimes you can have chemotherapy before surgery to shrink the cancer so that lumpectomy is possible.
- Removing all of the breast tissue. A mastectomy is surgery to remove all breast tissue from a breast. The most common mastectomy procedure is total mastectomy, also called simple mastectomy. This procedure removes all of the breast, including the lobules, ducts, fatty tissue and some skin, including the nipple and areola.Mastectomy might be used to remove a large cancer. It also might be needed when there are multiple areas of cancer within one breast. You might have a mastectomy if you can’t have or don’t want radiation therapy after surgery.Some newer types of mastectomy procedures might not remove the skin or nipple. For instance, a skin-sparing mastectomy leaves some skin. A nipple-sparing mastectomy leaves the nipple and the skin around it, called the areola. These newer operations can improve the look of the breast after surgery, but they aren’t options for everyone.
- Removing a few lymph nodes. A sentinel node biopsy is an operation to take out some lymph nodes for testing. When breast cancer spreads, it often goes to the nearby lymph nodes first. To see if the cancer has spread, a surgeon removes some of the lymph nodes near the cancer. If no cancer is found in those lymph nodes, the chance of finding cancer in any of the other lymph nodes is small. No other lymph nodes need to be removed.
- Removing several lymph nodes. Axillary lymph node dissection is an operation to remove many lymph nodes from the armpit. Your breast cancer surgery might include this operation if imaging tests show the cancer has spread to the lymph nodes. It also might be used if cancer is found in a sentinel node biopsy.
- Removing both breasts. Some people who have cancer in one breast may choose to have their other breast removed, even if it doesn’t have cancer. This procedure is called a contralateral prophylactic mastectomy. It might be an option if you have a high risk of getting cancer in the other breast. The risk might be high if you have a strong family history of cancer or have DNA changes that increase the risk of cancer. Most people with breast cancer in one breast will never get cancer in the other breast.
Complications of breast cancer surgery depend on the procedures you choose. All operations have a risk of pain, bleeding and infection. Removing lymph nodes in the armpit carries a risk of arm swelling, called lymphedema.
You may choose to have breast reconstruction after mastectomy surgery. Breast reconstruction is surgery to restore shape to the breast. Options might include reconstruction with a breast implant or reconstruction using your own tissue. Consider asking your healthcare team for a referral to a plastic surgeon before your breast cancer surgery.
Radiation therapy
Radiation therapy treats cancer with powerful energy beams. The energy can come from X-rays, protons or other sources.
For breast cancer treatment, the radiation is often external beam radiation. During this type of radiation therapy, you lie on a table while a machine moves around you. The machine directs radiation to precise points on your body. Less often, the radiation can be placed inside the body. This type of radiation is called brachytherapy.
Radiation therapy is often used after surgery. It can kill any cancer cells that might be left after surgery. The radiation lowers the risk of the cancer coming back.
Side effects of radiation therapy include feeling very tired and having a sunburn-like rash where the radiation is aimed. Breast tissue also may look swollen or feel more firm. Rarely, more-serious problems can happen. These include damage to the heart or lungs. Very rarely, a new cancer can grow in the treated area.
Chemotherapy
Chemotherapy treats cancer with strong medicines. Many chemotherapy medicines exist. Treatment often involves a combination of chemotherapy medicines. Most are given through a vein. Some are available in pill form.
Chemotherapy for breast cancer is often used after surgery. It can kill any cancer cells that might remain and lower the risk of the cancer coming back.
Sometimes chemotherapy is given before surgery. The chemotherapy might shrink the breast cancer so that it’s easier to remove. Chemotherapy before surgery also might control cancer that spreads to the lymph nodes. If the lymph nodes no longer show signs of cancer after chemotherapy, surgery to remove many lymph nodes might not be needed. How the cancer responds to chemotherapy before surgery helps the healthcare team make decisions about what treatments might be needed after surgery.
When the cancer spreads to other parts of the body, chemotherapy can help control it. Chemotherapy may relieve symptoms of an advanced cancer, such as pain.
Chemotherapy side effects depend on which medicines you receive. Common side effects include hair loss, nausea, vomiting, feeling very tired and having an increased risk of getting an infection. Rare side effects can include premature menopause and nerve damage. Very rarely, certain chemotherapy medicines can cause blood cell cancer.
Hormone therapy
Hormone therapy uses medicines to block certain hormones in the body. It’s a treatment for breast cancers that are sensitive to the hormones estrogen and progesterone. Healthcare professionals call these cancers estrogen receptor positive and progesterone receptor positive. Cancers that are sensitive to hormones use the hormones as fuel for their growth. Blocking the hormones can cause the cancer cells to shrink or die.
Hormone therapy is often used after surgery and other treatments. It can lower the risk that the cancer will come back.
If the cancer spreads to other parts of the body, hormone therapy can help control it.
Treatments that can be used in hormone therapy include:
- Medicines that block hormones from attaching to cancer cells. These medicines are called selective estrogen receptor modulators.
- Medicines that stop the body from making estrogen after menopause. These medicines are called aromatase inhibitors.
- Surgery or medicines to stop the ovaries from making hormones.
Hormone therapy side effects depend on the treatment you receive. The side effects can include hot flashes, night sweats and vaginal dryness. More-serious side effects include a risk of bone thinning and blood clots.
Targeted therapy
Targeted therapy uses medicines that attack specific chemicals in the cancer cells. By blocking these chemicals, targeted treatments can cause cancer cells to die.
The most common targeted therapy medicines for breast cancer target the protein HER2. Some breast cancer cells make extra HER2. This protein helps the cancer cells grow and survive. Targeted therapy medicine attacks the cells that are making extra HER2 and doesn’t hurt healthy cells.
Many other targeted therapy medicines exist for treating breast cancer. Your cancer cells may be tested to see whether these medicines might help you.
Targeted therapy medicines can be used before surgery to shrink a breast cancer and make it easier to remove. Some are used after surgery to lower the risk that the cancer will come back. Others are used only when the cancer has spread to other parts of the body.
Immunotherapy
Immunotherapy is a treatment with medicine that helps the body’s immune system to kill cancer cells. The immune system fights off diseases by attacking germs and other cells that shouldn’t be in the body. Cancer cells survive by hiding from the immune system. Immunotherapy helps the immune system cells find and kill the cancer cells.
Immunotherapy might be an option for treating triple-negative breast cancer. Triple-negative breast cancer means that the cancer cells don’t have receptors for estrogen, progesterone or HER2.
Palliative care
Palliative care is a special type of healthcare that helps you feel better when you have a serious illness. If you have cancer, palliative care can help relieve pain and other symptoms. A team of healthcare professionals provides palliative care. The team can include doctors, nurses and other specially trained professionals. Their goal is to improve quality of life for you and your family.
Palliative care specialists work with you, your family and your care team to help you feel better. They provide an extra layer of support while you have cancer treatment. You can have palliative care at the same time as strong cancer treatments, such as surgery, chemotherapy or radiation therapy.
When palliative care is used along with all of the other appropriate treatments, people with cancer may feel better and live longer.
What are treatment side effects?
Common chemotherapy and radiation therapy side effects include fatigue, nausea and vomiting. Targeted therapy, immunotherapy and hormone therapy have similar side effects, including gastrointestinal issues like constipation and diarrhea.
People react differently to breast cancer treatments. If you’re receiving treatment, ask your healthcare provider how treatment may affect you, including how it may affect your daily life.
Complications of breast cancer surgery
All surgeries have potential complications, and breast cancer surgery is no exception. As you’re considering your options, it’s important to remember that surgery removes potentially life-threatening cancer. In general, the risks of breast cancer outweigh the complications.
If you’re having breast cancer surgery, ask your healthcare provider to explain potential complications, which may include:
- Infection at the surgical site.
- Blood clots that can happen after surgery.
- Nerve damage.
- Lymphedema.
You can also read: Treatments of leukemia
Conclusion
Breast cancer occurs when breast cells develop mutations and begin to divide and multiply. Some people may notice symptoms such as a lump, discoloration, or texture changes.
There are several types of breast cancer, which are broken into two main categories: invasive and noninvasive. The type of cancer you have helps guide your treatment options and long-term outcome.
If you notice any changes to your breast, such as a lump, swelling, or pain, reach out to a healthcare professional for advice. They can run some tests to identify what could be causing your symptoms.
Remember, breast cancer survival rates are improving. The earlier the cancer is caught, the better your outlook may be.
- List of Common Diseases & Medical Disorders
- Buy Complete Premium Anatomy Notes (PDFs)
- Medmichihealthcare New posts
- Read All causes of disease short notes
- Read All diagnosis of disease short notes
- Read All treatment of disease short notes
- Subscribe Medmichihealthcare YouTube channel
Discover more from Medmichihealthcare
Subscribe to get the latest posts sent to your email.